Medical technology has advanced at an extraordinary pace to ensure patients receive treatment that is both safer and more effective. One of the most significant innovations is the Da Vinci Surgical Robot, acutting-edge robotic system designed to assist surgeons in minimally invasive Surgeries (MIS). It enhances accuracy in hard-to-reach areas and significantly reduces trauma to the patient’s body.
The Da Vinci Robot-Assisted Surgery is approved by the U.S. Food and Drug Administration (FDA) and is now used in leading hospitals worldwide. With millions of successful procedures performed to date, it continues to demonstrate strong, reliable clinical outcomes.
What is the Da Vinci Surgical Robot?
The Da Vinci system is a computer-assisted robotic device with four robotic arms capable of movements far more delicate and precise than the human hand.
Surgeons operate the system via a dedicated console, viewing the surgical site in enhanced, high-definition 3D. Every hand movement is transmitted in real time to miniature instruments inside the patient’s body, supported by motion-stabilizing technology that eliminates natural hand tremors. This enables highly precise operations even in complex anatomical areas.
How Does the Da Vinci System Work?
The Da Vinci system operates in harmony with the surgeon and consists of three core components:
1) Surgeon Console
The surgeon sits at a console, viewing the surgical field in high-resolution 3D. Hand and finger movements are transmitted into precise robotic instrument motions inside the patient.
2) Patient-side cart
The patient-side unit includes four robotic arms—one for the camera and three for surgical instruments. These arms can articulate and rotate far beyond the limits of the human wrist, allowing access to deep or narrow spaces while minimizing disruption to surrounding tissues.
3) Vision System
The visual cart provides magnified, high-definition 3D visuals, delivering exceptional clarity of tissues, vessels, and structures for safer and more confident surgical decision-making.
Key Advantages of the Da Vinci Surgical Robot
- High-definition 3D visualization for enhanced clarity
- Articulating robotic arms that move with exceptional flexibility
- Reduced trauma to the surrounding tissue and less blood loss
- Smaller incisions, less postoperative pain, and faster recovery
- Lower risk of complications
- High precision facilitates surgeons in the most delicate procedures
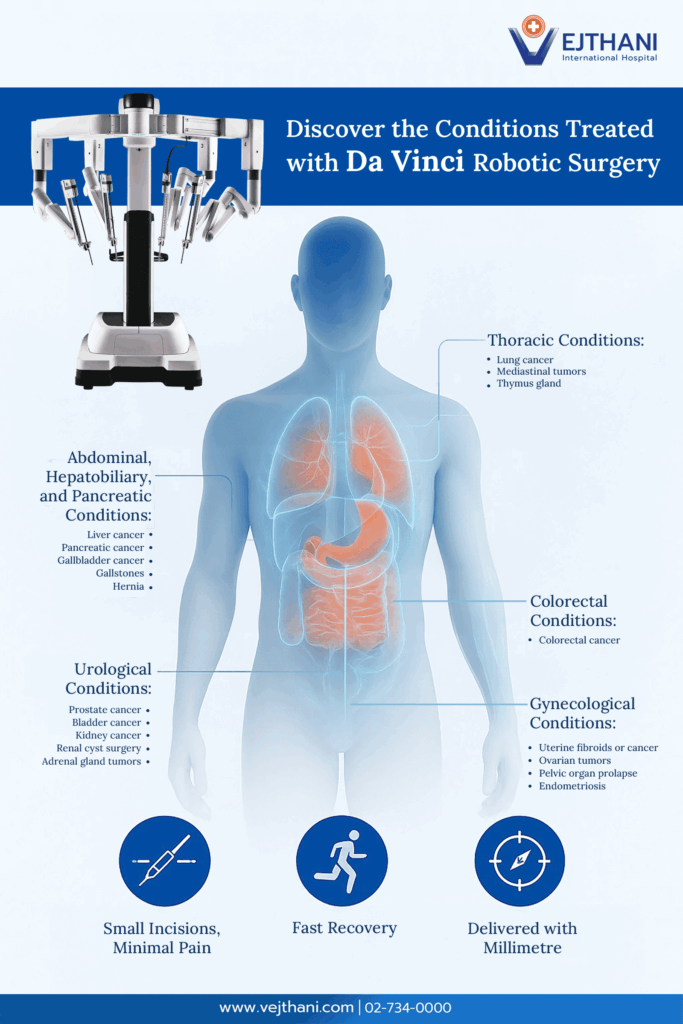
Which Conditions Can be Treated with Da Vinci Robot-Assisted Surgery?
The Da Vinci Surgical Robot is used across multiple specialties, particularly in complex cases.
Urological Conditions
- Prostate cancer
- Malignant tumors or abnormal tumors in the kidney, bladder, or adrenal glands
Abdominal, Hepatobiliary, and Pancreatic Conditions
- Hernia
- Liver cancer, pancreatic cancer, gallbladder cancer
- Gallstones
- Tumors in the bile duct or pancreas
Gynecological Conditions
- Uterine fibroids and ovarian tumors
- Uterine cancer
- Endometriosis
- Pelvic organ prolapses
Colorectal Conditions
Thoracic Conditions
- Lung cancer
- Tumors in the mediastinum
The Da Vinci Robot-Assisted Surgery enhances surgical outcomes by reducing trauma, promoting faster recovery, and improving precision compared to traditional open surgery—helping patients achieve safer and better long-term results under expert medical care.
Frequently Asked Questions (FAQ)
What is the Da Vinci Surgical Robot?
The Da Vinci Surgical Robot is a computer-controlled robotic system with four highly flexible arms. Surgeons operate it through a 3D high-definition console, enabling smaller incisions, greater accuracy, and reduced impact on the body.
How is Da Vinci surgery better than conventional surgery?
Key benefits include:
- Smaller incisions, less pain, faster recovery
- Magnified 3D visualization
- Minimal damage to surrounding tissues and less blood loss
- Enhanced precision and reduced risk of complications
Which medical conditions are suitable for treatment with Da Vinci Robotic-Assisted Surgery?
It is ideal for complex procedures in:
- Urology (e.g., prostate cancer)
- Abdominal and hepatobiliary conditions (e.g., liver cancer, gallstones)
- Gynecology (e.g., fibroids, endometriosis)
- Colorectal cancer
- Thoracic surgery (e.g., lung cancer)
For more information, please contact
Surgery Center, Vejthani International Hospital
Call: (+66)2-734-0000 Ext. 4500, 4501
English Hotline: (+66)85-223-8888