Overview
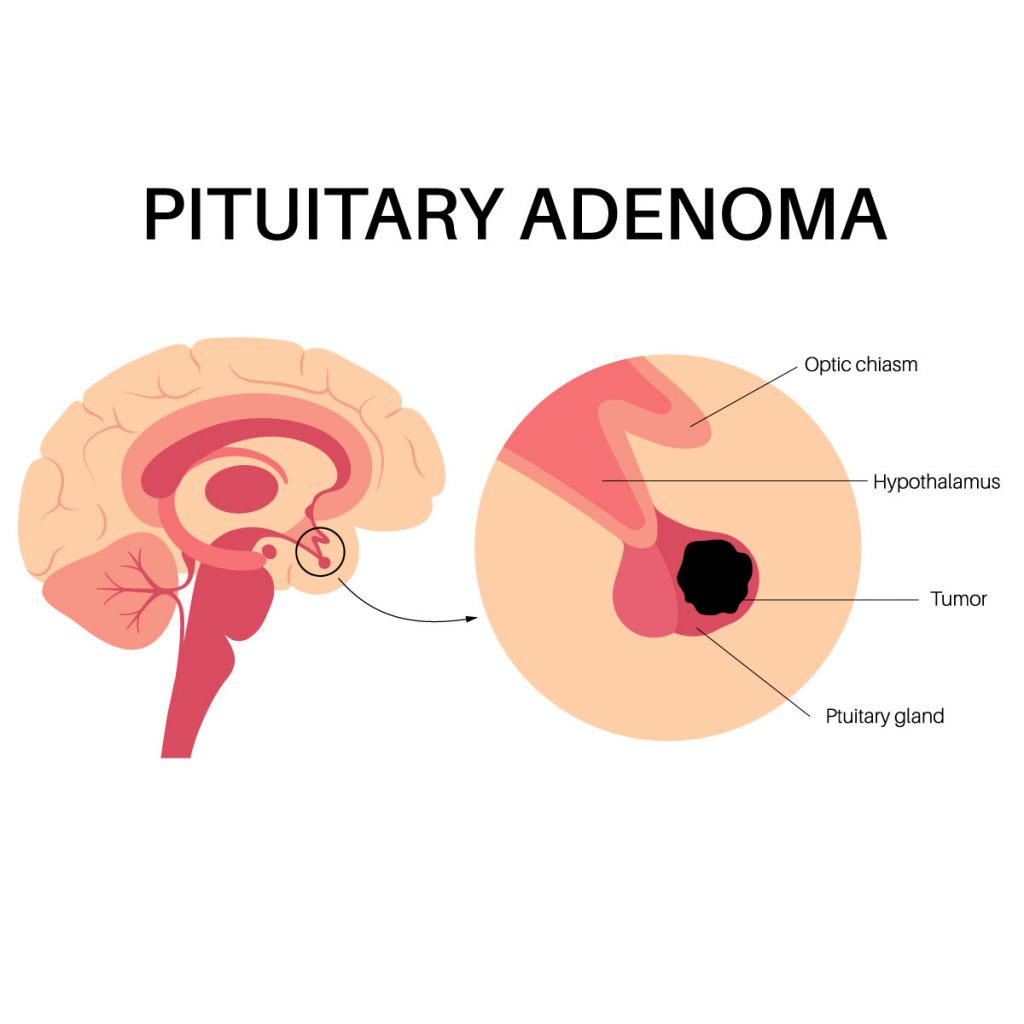
The abnormal growth of tumor that occur at the pituitary gland is called pituitary tumor. The pituitary gland is a small gland that is about the size of a pea, it connects to the hypothalamus, just behind the nose. It has two lobes, the anterior lobe and posterior lobe that releases different hormones.
Pituitary adenomas are noncancerous type of tumor and doesn’t spread to other parts of the body, however they could pose a risk in the functionality of the pituitary gland and cause risk to the health. Pituitary gland’s ability to produce hormones may be affected by some pituitary tumors. Hormones that control vital bodily processes are produced in excess by some pituitary tumors.
There are different kinds of treatment for pituitary tumors, such as surgical removal of the tumor, and medications to control hormone levels. It is recommended to have a consultation with the specialist for proper diagnosis.
Categories of pituitary adenomas according to secretion:
- Functioning adenomas (secreting): Pituitary tumors can produce an excessive level of hormones. Functional adenomas includes:
- Prolactinoma: a tumor that overproduces prolactin.
- Somatotroph adenoma: a tumor that overproduces growth hormone that will cause acromegaly.
- Corticotroph adenoma: a tumor that overproduces adrenocorticotropic hormone (ACTH) that cause will Cushing’s syndrome.
- Thyrotroph adenomas: a tumor that overproduces thyroid-stimulating hormone (TSH) that will cause hyperthyroidism.
- Gonadotroph adenomas: a tumor that overproduces gonadotropin hormones.
- Nonfunctioning adenomas (non-secreting): Pituitary tumors that do not produce any hormones. But if they become large, they can become mass effect and compress nearby structure.
Categories of Pituitary adenomas according to size:
- Microadenomas: Their size is smaller than 10 millimeters.
- Macroadenomas: Their size is over 10 millimeters. Macroadenomas occur as common compared to microadenomas. They are also more likely to result in hypopituitarism, which is characterized by lower hormone level compared to normal.
Symptoms
Some pituitary glands do not show any signs or symptoms. Depending on the production of hormone, pituitary tumors that are functioning might result in a different kind of signs and symptoms. Occasionally the pituitary tumors are discovered by incidental finding during an imaging examination like an MRI or CT that was done for another purpose. Pituitary tumors that are growing and putting pressure on other structures are related to the signs and symptoms of non-producing hormones (nonfunctioning) pituitary tumors.
Signs and symptoms (tumor pressure)
The following signs and symptoms result from the large size tumor’s pressure on the pituitary tumor:
- Vision problems
- Headaches
Signs and symptoms (hormonal deficiency)
Pituitary macroadenomas can harm the tissue of the pituitary gland, which can result in one or more pituitary hormone deficits. Hypopituitarism, or an underactive pituitary gland, may occur and present with the following symptoms.
- Luteinizing Hormone (LH) and Follicle Stimulating Hormone (FSH) deficiency: hypogonadism, a condition marked by low levels of both estrogen (FSH) and testosterone (LH), results.
- Hot flashes
- Vaginal dryness
- Erectile dysfunction in men
- Reduced facial/body hair development in male.
- Mood swings
- Loss of libido
- Thyroid Stimulating Hormone (TSH) deficiency: condition marked by low thyroid hormone production called hypothyroidism with the following symptoms:
- Fatigue or weakness
- Constipation
- Slow heartbeat
- Dry skin
- Swelling of extremities
- Slower reflexes.
- Adrenocorticotropic hormone-secreting (ACTH) deficiency: is a decrease in cortisol production which called adrenal insufficiency. Symptoms are the following:
- Low blood pressure
- Nausea and vomiting
- Abdominal pain
- Poor appetite.
- Growth Hormone deficiency: low production of growth hormone. Symptoms depend on the age of the patient.
- Fatigue
- Weakness
- Decrease in the muscle mass
Signs and symptoms (overproduction of hormone)
Some pituitary adenoma overproduce one or more pituitary hormones, known as hyperpituitarism. The symptoms of hyperpituitarism vary depend on the affected hormones.
- Adrenocorticotropic hormone-secreting (ACTH) tumors: is an increase in cortisol production which called Cushing syndrome. Symptoms are the following:
- Rounded face
- Increased fat around the neck
- High blood pressure
- High blood sugar
- Purple stretch marks over the belly
- Easy bruising
- Muscle weakness
- Osteoporosis
- Growth hormone-secreting tumors (somatotroph adenoma): excessive secretion of growth hormone. Symptoms depend on the age of the patient.
- In adult, excessive secretion of growth hormones cause a condition called acromegaly. Symptoms are the following:
- Joint aches and pain
- Enlarged hands and feet
- Excessive sweating
- Heart problems
- Facial changes
- In children, excessive secretion of growth hormones causes a condition called gigantism. Symptoms are the following:
- Gaps between the teeth
- Large hands and feet
- Enlargement of the forehead, jaw, and nose
- In adult, excessive secretion of growth hormones cause a condition called acromegaly. Symptoms are the following:
- Prolactin-secreting tumors: pituitary tumor that causes excessive secretion of prolactin called prolactinoma. This result in a decreased level of sex hormones.
- In women, prolactinoma can cause:
- Irregular menstrual period or no menstrual period
- Milk discharge from breast (when not pregnant/breast feeding)
- In men, prolactinoma can cause:
- Loss of interest in sexual activity
- Enlarged breast
- Decreased sperm production
- In women, prolactinoma can cause:
- Thyroid-stimulating hormone-secreting tumors: excessive secretion of thyroid-stimulating hormone (TSH) causes a condition called hyperthyroidism. Symptoms are the following:
- Unexplained weight loss
- Rapid heartbeat
- Excessive sweating
- Irritability
Consult the doctor if patient experience any signs or symptoms that could point to a pituitary tumor. Pituitary tumors are frequently treatable, allowing your hormone levels to return to normal and reducing its symptoms.
Talk to the doctor about routine testing that could aid in the early detection of a pituitary tumor if multiple endocrine neoplasia type 1 (MEN 1) runs in the family.
Causes
It is unclear what causes the pituitary gland’s uncontrolled cell development, which results in tumors.
A small, bean-shaped gland called the pituitary gland is found at the base of the brain, between the ears and behind the nose. The gland affects the functioning of the body despite its small size. It generates hormones that control vital processes like growth, blood pressure, and reproduction.
Most cases of pituitary tumors lack any obvious hereditary component, while a small percentage run in families. The development of pituitary tumors is thought to be significantly influenced by genetic changes.
Risk factors
A higher risk of pituitary tumor exists in those who have a family history of specific genetic diseases. Additional hereditary disorders linked to pituitary adenomas include:
- Multiple endocrine neoplasia type 1 (MEN 1)
- Multiple endocrine neoplasia type 4 (MEN 4)
- Neurofibromatosis type 1
- Carney complex
- X-LAG syndrome
- Succinate dehydrogenase-related familial pituitary adenoma
- Von Hippel-Lindau syndrome
Diagnosis
Depending on the type of tumor the patient have and whether it cause symptoms or not, the diagnostic procedure for pituitary adenomas will vary, and due to the symptoms similarity to those of other illnesses, pituitary tumors often go undetected.
Sometimes, medical examinations for other illnesses lead to the discovery of pituitary tumors.
Specialist will perform a physical examination as well as gather the medical history to determine whether the patient has a pituitary tumor. The specialist may recommend the following test:
- Blood tests: Pituitary tumor can be diagnosed using blood tests that measure the levels of hormonal abnormalities associated with pituitary tumors.
- Urine tests: used to identify breakdown products of hormone processing in your body
- Imaging tests: To determine the location and size of the tumor, the specialist may recommend imaging tests of the brain. Imaging test includes.
- Magnetic Resonance Imaging (MRI) scan that creates a thorough, 3-D image of the brain and surrounding tissue using a magnet and radio waves.
- Computerized tomography (CT) with series of images are captured. The specialist can assess how the pituitary tumor may be affecting patients by creating a thorough view of it using the photographs on a computer.
- Vision testing: To check if the sight or peripheral vision of the patient has been affected by pituitary tumor.
Treatment
Treatment is not necessary for most pituitary tumors. If the patient has a tumor, the type, size, and depth to which it has spread will determine the treatment. The age and general health are additional considerations.
A multidisciplinary approach will be recommended, which involves specialist from different field, ENT surgeon, neurosurgeon, endocrinologist, and oncologist (radiation). To remove a pituitary tumor and restore normal hormone production, doctors typically utilize surgery, radiation therapy, and drugs, either individually or in combination.
Medications
Medication may assist to reduce various forms of pituitary tumors and stop excessive hormone secretion:
- Prolactin-secreting tumors (prolactinomas): This drug decreases prolactin secretion and reduces the size of the tumor. The use of cabergoline and bromocriptine will be closely monitored. Possible side effects of these drug includes dizziness, nausea, drowsiness, diarrhea, constipation, and depression.
- ACTH-producing tumors (Cushing syndrome): This drug reduces the adrenal gland’s excessive cortisol production. The use of ketoconazole, mitotane and metyrapone will be closely monitored. Osilodrostat also decreases the production of cortisol. Pasireotide reduces the amount of ACTH produced by a pituitary tumor. Possible sign effect of these drug include nausea, diarrhea, high blood pressure, and weakness.
- Growth hormone-secreting tumors: These kinds of pituitary tumors can be treated with two different types of medications, which are especially helpful if surgery hasn’t been able to restore normal growth hormone production. Somatostatin analogs like octreotide and lanreotide reduce the synthesis of growth hormone, which may cause the tumor to shrink. The second class of medication, pegvisomant, prevents the body from being affected by too much growth hormone. Possible side effect of these drug include nausea, vomiting, headache, and stomach pain.
Radiation therapy
Tumors are eliminated by radiation therapy using high-energy radiation. If surgery is not a possibility, radiation can be done alone. If a tumor remains after surgery or recurs and creates signs and symptoms that drugs are unable to treat, radiation therapy may be helpful. Among the radiation therapy techniques are:
- Stereotactic radiosurgery: radiation beams are focused on the tumor without making an incision and are frequently administered as a single high dose. The risk of damaging normal tissue is reduced since little radiation interacts with the healthy tissue surrounding the tumor. With the use of specialized brain imaging tools, radiation beams are delivered directly onto the tumor.
- External beam radiation: This gradually releases radiation in little doses which takes a long time to stop the tumor growth. Radiation therapy has the potential to harm healthy brain tissue and any remaining normal pituitary cells, especially in areas close to the pituitary gland.
- Intensity modulated radiation therapy (IMRT): With the use of a computer, the physician can utilize this form of radiation therapy to shape the beams and surround the tumor from a different angle. Additionally, the beams’ intensity can be controlled, which will reduce the amount of radiation that reaches nearby tissues.
- Proton beam therapy: This type of radiation uses positively charged ions (protons). Proton beams release their energy inside onto the tumor. The beams can be precisely regulated and can be applied to tumors with little harm to healthy tissues.
Surgery
Pituitary tumors that are pressing on the optic nerves or that are overproducing hormones, will be surgically removed. The type of tumor, its location, size, and if it has spread to surrounding tissues all determine the outcome of the surgery. Pituitary tumors can be treated surgically using two main methods:
- Endoscopic transnasal transsphenoidal approach: This will allow the surgeon to remove the tumor without making an external incision by going through the nose and sinus. The brain will be unaffected, and no scar will be visible. This procedure may difficult to remove large tumors, especially if the tumor has spread to surrounding nerves or brain tissue.
- Transcranial approach (craniotomy): A scalp incision is used to remove the tumor from the upper part of your skull. This approach makes it simpler to access larger or more difficult tumors.
Replacement of pituitary hormones
To maintain normal hormone levels, patient need to take replacement hormones if a pituitary tumor is found or surgery to remove it that reduces hormone production. Replacement pituitary hormones are necessary for some radiation patients.
Observation
If the patient decides to observe for a certain period of time prior to treatment, routine follow-up examination to see if the tumor has grown will be required. If the tumor isn’t causing any symptoms or signs, this can be a choice of treatment.
If the pituitary tumor isn’t creating additional issues, many patients manage without treatment. For younger patients, observation is recommended but the patient must understand that the tumor could change or develop while being observed. Patient could discuss with the specialist for possible symptoms and potential treatment.





