Overview
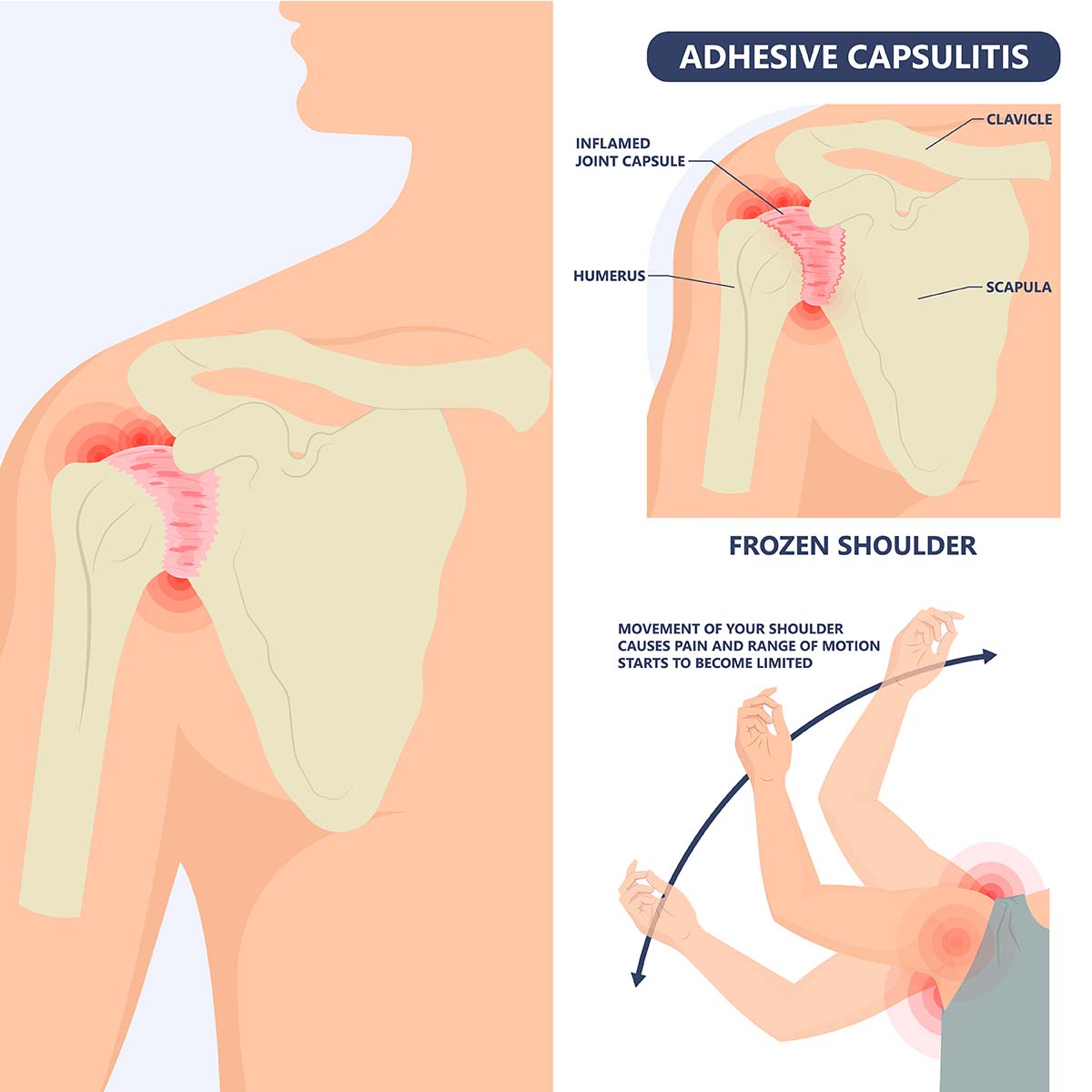
If you are experiencing shoulder joint pain and stiffness, you are having a condition called frozen shoulder or also called adhesive capsulitis. This condition begins to have symptoms gradually and worsens over time until it resolves within a year or three.
Immobility of the arm from a medical condition recovery such as post-stroke or after a procedure like undergoing a mastectomy increases the risk of having a frozen shoulder.
Recurrence of frozen shoulder in the same side is less common, although the opposite shoulder may develop the same condition.
Symptoms
There are three stages of frozen shoulder and each of these stages can last for months.
- Freezing stage. The range of motion of the shoulder becomes limited and any movement results to pain.
- Frozen stage. At this stage, the pain can be less but the shoulder movement is difficult because it has become stiffer.
- Thawing stage. This stage shows an improvement in shoulder motion.
The pain can get worse in the evening which affects the quality of sleep in some people.
Causes
Frozen shoulder happens when the shoulder’s capsule which encases the tendons, ligaments and bones thickens and tightens around the shoulder joints, which results to movement limitation.
The reason is uncertain, but it is more common in diabetics or people who needs to immobilize their shoulders for a long time (e.g. arm fracture or post-surgery condition).
Risk factors
The following may increase your risk of having a frozen shoulder:
- Age and sex. If you are 40 years old or more, especially if you are a woman, you are most likely to develop a frozen shoulder.
- Inability to move or reduced movement. A long period of immobility or reduced movement of the shoulder poses a higher risk of developing frozen shoulder which can be caused by:
- Rotator cuff injury
- Fractured arm
- Stroke
- Surgery recovery
- Systemic diseases. The following diseases increases the risk of having frozen shoulder:
- Cardiovascular disease
- Diabetes
- Tuberculosis
- Parkinson’s disease
- Hyperthyroidism
- Hypothyroidism
Diagnosis
Certain movements and muscle relaxation will be instructed to you by the doctor in order to assess your range of motion and pain, or inject an anesthetic or numbing medicine. Both active and passive range of motion can be affected by a frozen shoulder.
Your signs and symptoms can diagnose a frozen shoulder but diagnostic tests such as an X-ray or Magnetic Resonance Imaging (MRI) might be recommended to confirm it.
Treatment
The following treatment can be done to alleviate the pain and conserve the shoulder’s range of motion:
Shoulder exercises
Exercises that will control the shoulder pain and conserve its range of motion can treat frozen shoulder.
Medications
Over-the-counter pain relievers to reduce pain and inflammation.
Therapy
range-of-motion exercises as taught by physical therapist to help optimize and recover mobility.
Surgical and other procedures
Frozen shoulder mostly resolves on its own within a year up to 18 months. If symptoms persist, the doctor may recommend:
- Steroid injections. Improves shoulder mobility and reduces pain, especially if received in an earlier stage.
- Joint distension. Sterile water injection to the joint capsule to mobilize the joint and stretch the tissue.
- Shoulder manipulation. A general anesthesia is given by the doctor so you will unconscious and not feel the pain. The doctor then loosens the tightened tissue by moving the shoulder joints in various directions.
- Surgery. It is uncommon to perform surgery for a frozen shoulder but if everything else fails, surgery may be recommended by the doctor. The surgery removes scar tissues and adhesions inside your shoulder joint and is usually done by arthroscopically.
Lifestyle and home remedies
It is best to use or move the affected shoulder based on your pain or range of motion limitations. Heat or cold compress can also relieve the pain.





