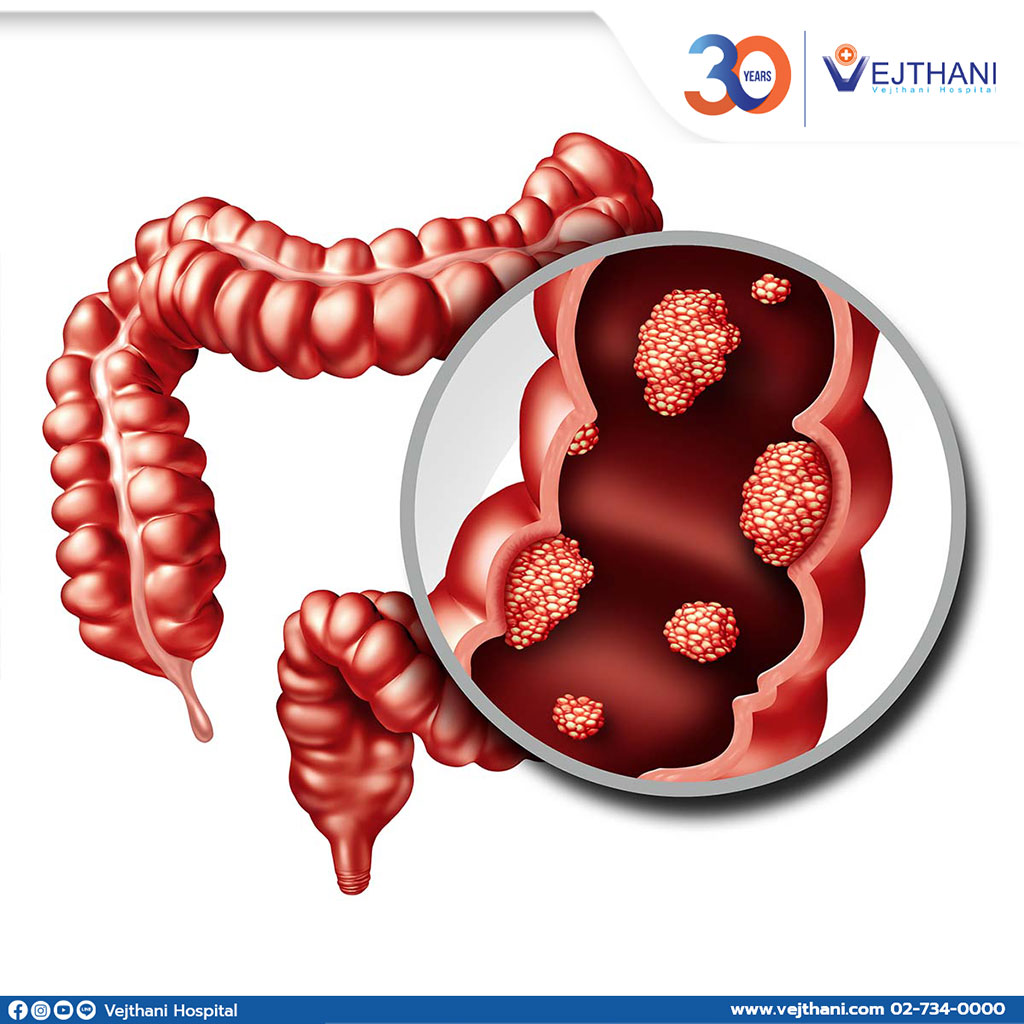
Cancer that initially develops in the large intestine (colon) is called colon cancer. Colon is the last part of the digestive tract.
Colon cancer is commonly found in elders. However, patients of any age can have the disease. Colon cancer generally starts with small, noncancerous accumulations of cells, known as polyps. These occur on the inside of the colon. As time progresses, these polyps can develop into colon cancers.
Most patients with colonic polyp are asymptomatic. Therefore, regular screening tests are recommended in order to prevent colon cancer by detecting and removing polyps before they develop into cancer.
Treatment options for colon cancers are surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy.
Colon cancer is also known as colorectal cancer. The term implies the combination of colon cancer and rectal cancer, which starts in the rectum.
Signs and symptoms
- A constant change in the bowel habits such as diarrhea, constipation
- Change in stool consistency
- Rectal bleeding, dark stool or blood in the stool
- Continuous abdominal discomfort such as cramps, bloatingor pain
- A feeling of incomplete bowel
- Fatigue or weakness
- Unexplained weight loss
Early-stage of colon cancer is usually asymptomatic until the disease has progressed to the late stage.
Causes
The definite causes of colon cancer are unknown. The mutation in DNA of colon cells causes uncontrolled duplication resulting in forming a mass of cells also known as a tumor. This tumor then begins to invade and destroy the healthy cells and tissues. These cells have the tendency to metastasize (spread to other parts of the body).
Risk factors
- Age. Colon cancer tends to be found in patients of any age but most of the people who have been diagnosed are above 50 years. Nevertheless, the percentage of colon cancer detected in people younger than 50 years old is rising.
- African-American race. African-American has a higher risk of developing colon cancer.
- Personal record of colorectal cancer or polyps. Having colon cancer or noncancerous colon polyps previously increase the risk of getting colon cancer in the future.
- Inflammatory intestinal conditions. Having chronic inflammatory diseases such as ulcerative colitis and Crohn’s disease, raises the chance of getting colon cancer.
- Inherited syndromes. Certain gene mutations pass down to generations which puts a greater risk in developing colon cancer. The syndromes include familial adenomatous polyposis (FAP) and Lynch syndrome, which is also known as hereditary nonpolyposis colorectal cancer (HNPCC).
- Family history of colon cancer. People with a first-degree relative (parent, sibling, or child) with colon cancer increase the risk of developing colon cancer. If more than one family member has colon cancer or rectal cancer, your risk is even greater.
- Low-fiber and high-fat diet. This kind of diet could put patients at risk of developing colon cancer and rectal cancer. Certain studies have revealed that high consumption of red meat and processed meat could also be a contributing factor for colon cancer to occur.
- Inactive lifestyle. People living a sedentary lifestyle are likely to have colon cancer. Consistent physical activities may decrease the chance of developing the disease.
- Diabetes. Diabetic patients or people who are resistant to insulin are at great risk of colon cancer.
- Obesity. Being obese puts patients at risk of colon cancer
- Smoking. Smoking increases the risk of having colon cancer.
- Alcohol. Heavy consumption of alcohol raises the risk of getting colon cancer.
- Radiation therapy for cancer. Radiation therapy applied to the abdomen for previous cancer treatment increases the chance of having colon cancer.
Diagnosis
Screening
Different screening tests are recommended to different group of people. The advantage of detecting colon cancer at the earliest stage gives patients a significant chance of being cured. Some screening tests aim to find polyps or noncancerous colon polyps, which are advised to healthy people who have no symptoms. There has been some evidence that screening tests can reduce the risk of death from colon cancer.
Approximately people at the age of 45 are recommended to start colon cancer screening tests. People with family history of having colon cancer or African-American are advised to do the screening sooner as they are at higher risk.
Diagnosing
One or more of the following tests may be recommended if patients have symptoms of colon cancer:
- Colonoscopy is an investigation consisting of flexible thin tube connected to a tiny camera which will be inserted into a patient’s bowel to evaluate at colon and rectum. If any unusual signs are detected, surgical tools will be inserted through the scope to collect tissue samples for analysis and polyps removal.
- Blood tests are not able to determine if a patient has colon cancer, however it will be done to obtain the health condition of the patients, such as kidney and liver function.
Carcinoembryonic antigen or CEA is a type of chemical produced by colon cancer. A test can be carried out to track the level of CEA in the body. This will help doctors to understand the chances of cure and determine how treatments are responding to cancers.
Determining the extent of the cancer
After being diagnosed with colon cancer, further tests will be advised to detect the stage of the disease. The type of treatment options that will be used to treat depends on the stage of the cancer. Therefore, staging is important in determining the most accurate treatment method for the patients. The tests to determine the stage of the cancer can be done through imaging procedures such as CT scans of abdomen, pelvic and chest.
Roman numerals from 0 to IV are indications of colon cancer stage. The lowest stage is when the cancer is only at the lining of the inside of the colon. In stage IV or advanced stage, the cancer has spread or metastasized to other parts of the body.
Treatment
Locations of the cancer, its stage and other health condition will determine the type of treatment. Generally, surgical removal of the cancer is the treatment for colon cancer. Radiation therapy and chemotherapy could also be used.
Surgery for early-stage colon cancer
- Removing polyps (polypectomy) during a colonoscopy if the cancer is small, has not spread and only exist within the polyp.
- Endoscopic mucosal resection is used to remove larger polyps during colonoscopy. Special tools can help remove the polyp and a tiny part of the inner lining of the colon.
- Minimally invasive surgery is done to remove the polyps that cannot be operated during colonoscopy. This operation is done by making a few small incisions in the abdominal wall, while medical equipment that has cameras attached will be inserted. The display of the colon will be shown on the monitor. Some samples may be collected from the lymph nodes that the cancer exist.
Surgery for more advanced colon cancer
- Partial colectomy is a surgical procedure that remove the part of colon that has cancer. A part of normal tissue on each side of the cancer will also be operated. The healthy part of the colon will be reconnected to the rectum later. Partial colectomy can be performed using a minimal invasive approach (Laparoscopy).
- Ostomy is done when it’s not possible to reconnect the colon or rectum. It is a surgical procedure that creates a way for waste to exit the body. It requires opening in the abdominal wall, where the remaining colon is located. Ostomy in certain cases are temporary while letting the colon and rectum to heal after surgery. Colostomy in some cases could be permanent.
- Lymph node removal is done during colon cancer surgery and sent for further investigation.
Surgery for advanced cancer
In cases where cancer is at an advanced stage or the patient has declined health condition, a procedure to release blockage in the colon will be advised to improve the symptoms. This operation is not designed to cure cancer, but to relieve symptoms like a blockage, bleeding or pain.
When cancer has spread only to the liver or lung while patient’s health condition is well, a surgery or other treatments that are localized can be done to eliminate the cancer. After or before this procedure, chemotherapy could be used in parallel for treatment. This treatment option results in the chance of being free from cancer in the long run.
Chemotherapy
Chemotherapy drugs to kill cancer cells. When treating colon cancer, chemotherapy is used after the surgical procedure when the cancer covered a large area and has invaded lymph nodes. Chemotherapy will then kill cancer cells that are left in the body and this diminishes the risk of cancer to reoccur.
Chemotherapy has the benefits of shrinking cancers that cover a broad area before the surgery as it becomes easier to operate the cancer.
Some symptoms of colon cancer cannot be eliminated by operation or when it has metastasized, this is when chemotherapy is used. Chemotherapy can also be given with the combination of radiation therapy.
Radiation therapy
Radiation therapy is the use of high-powered beams of energy sources,similar to X-rays and protons to destroy cancer cells. It has the ability to shrink big cancer so using it before a surgery, makes it easier to operate. If surgery is not a treatment option for the patient, radiation therapy will be given to relieve painful symptoms.
Targeted drug therapy
Targeted drug treatments particularly attack abnormalities that exist in the cancer cells. When the abnormalities are blocked, cancer cells die from the effect of targeted drug treatments.
Targeted drugs are often times given with the combination of chemotherapy and primarily given to patients who are at advanced stage of colon cancer.
Immunotherapy
Immunotherapy is a type of drug that relies on the function of immune system to fight cancer. The immune system in the body may not naturally fight against cancer because the cancer cells create proteins, which cannot be detected by the immune system. Immunotherapy interferes with this natural process. Advanced stage of colon cancer patients are commonly treated with immunotherapy. Sometimes cancer cells are tested prior to receive the medication to ensure the body will respond to the treatment.




