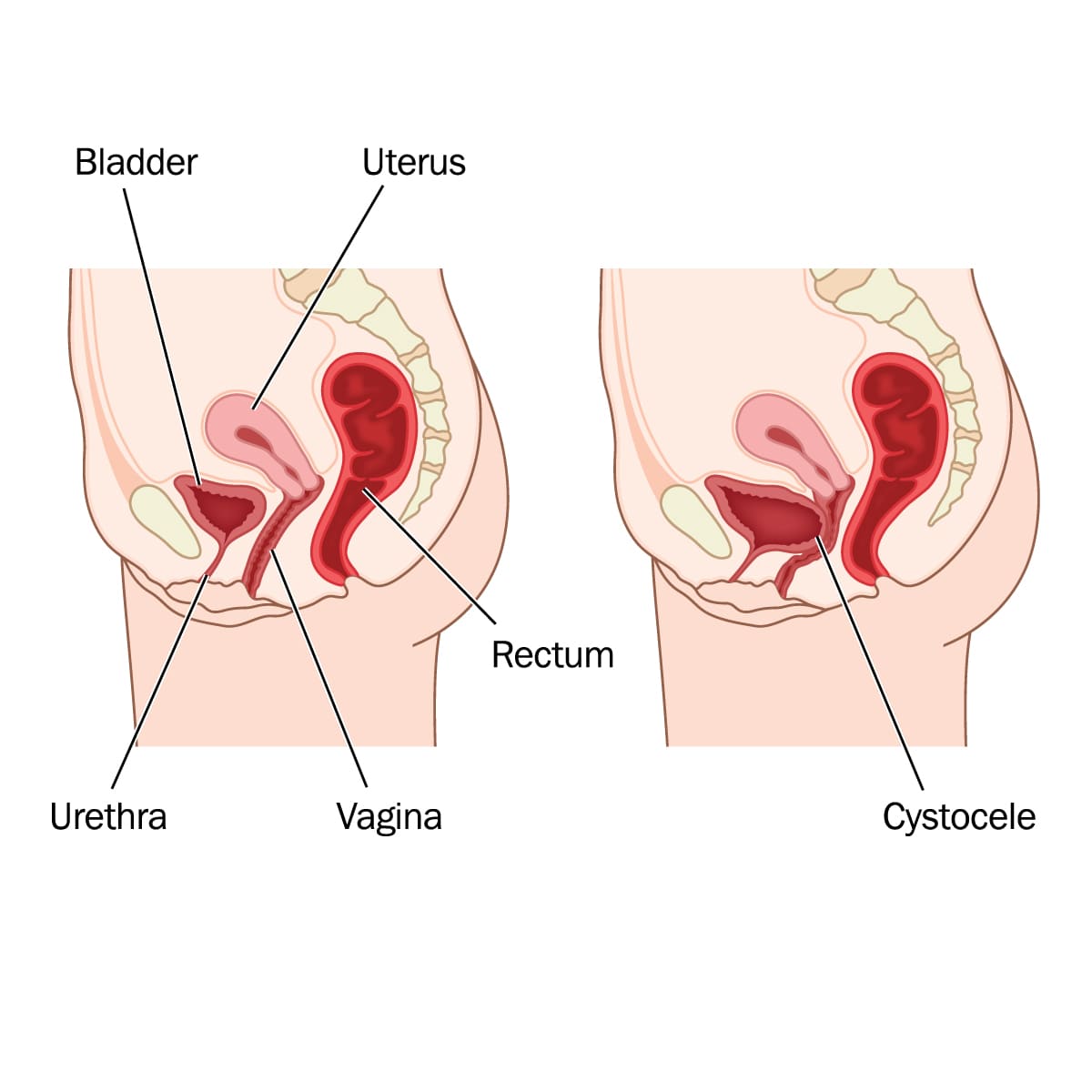
Anterior vaginal prolapse (Cystocele)
Overview
A cystocele occurs when the bladder falls from its normal position into the pelvic and pressing against the vaginal wall. It is often referred to as an anterior vaginal prolapse, herniated or a prolapsed bladder.
The muscles and connective tissues of the pelvic floor normally hold the organs of the pelvis, including the bladder, uterus, and intestines. Vaginal childbirth, chronic constipation, chronic coughing, or heavy lifting can increase the risk of cystocele, and which causes the pelvic floor to weaken or stretches that could lead to cystocele.
Many treatments are available for cystocele. Nonsurgical treatment is frequently successful for a mild or moderate prolapse. In severe prolapse, to retain the vagina and other pelvic organs in their normal locations, surgery may be required.
A grading or staging method is typically used by doctors to evaluate the severity of cystocele.
- Grade 1: The bladder only partially enters the vagina. This grade is considered mild.
- Grade 2: The bladder drops and almost reaching the vaginal opening. This is moderate case.
- Grade 3: The bladder reaches the vaginal opening and causes bulging. This is a severe case.
Symptoms
The patient might not experience or feel any symptoms or see any signs of cystocele. When they appear, signs and symptoms may include:
- Pelvic and vaginal pressure or fullness
- Feeling a bulge in the vagina
- Feeling of pelvic pressure during strain, cough, bear down or lift
- Urinary incontinence
- Constant need to urinate
- Recurring urinary tract infection
These symptoms may get worse when the patient is standing for a long time, heavy lifting, and coughing. The symptom will be relief when the patient is lie down. Prolapsed bladder could cause inconvenience and if it is left untreated it could lead to bladder infection. If the patient experiences any symptoms or signs that disturbs or interfere with their daily activities, it is recommended to schedule a visit with a healthcare professional.
Causes
The muscles, ligaments, and connective tissues that make up the pelvic floor support the bladder and other pelvic organs may get looser over time, due to delivery trauma, or of persistent pressure. The bladder may then drop lower than usual and protrude into the vagina.
The factors that contribute to weakening of pelvic floor include:
- Pregnancy and vaginal childbirth
- History of pelvic surgery (ex: hysterectomy or pelvic organ prolapse repair)
- Obesity or overweight
- Frequent heavy or intense lifting
- Straining with bowel movements
- Frequent coughing or bronchitis
Risk factors
The following factors contribute to the increased the risk to develop cystocele:
- Pregnancy and childbirth: Anterior prolapse is more likely to occur in women who have had vaginal or instrument-assisted deliveries, numerous pregnancies, or pregnancies with large-for-gestational-age babies.
- Aging: As the person gets older the body produces less estrogen, particularly after menopause, which results to weakening of pelvic floor.
- Hysterectomy: In some cases, surgical removal of the uterus could weaken of the pelvic floor.
- Genetics: Some women are more prone to anterior prolapse because of problems at birth such as weaker connective tissues.
- Obesity: Obese or overweight women are more likely to experience anterior prolapse.
Diagnosis
The healthcare provider will perform physical assessment and pelvic examination and further investigation to diagnose a cystocele:
- Pelvic examination: A tissue protrusion into the vagina during the examination could be a sign of pelvic organ prolapse. To proper evaluate the prolapse, the doctor will ask the patient to bear down as though during a bowel movement, and contract the pelvic floor muscles, like stopping the flow of urine to measure the strength of these muscles.
- Bladder and urine tests: The tests will determine how fully and effectively the bladder empties. The tests will show if the patient is holding more urine in the bladder than is typical even after emptying the bladder. The doctor may also do a test on a urine sample to investigate for signs of a bladder infection.
- Cystourethrogram: An X-ray of the bladder was taken while the woman was urinating and contrast dye will be injected into the bladder and urethra. It shows the bladder’s shape and any obstructions.
Treatment
If the cystocele has no symptoms or does not affect the quality of life, treatment is not necessary. The doctor may require a few clinic visits to monitor if the condition progresses or not.
If the cystocele has symptoms, the treatment will depend on its severity and any associated disorders, such as urinary incontinence or several types of pelvic organ prolapse.
Nonsurgical treatment:
- Kegel exercises: also called pelvic floor muscle exercise training, are structured routines that helps the pelvic floor muscles to become stronger. This enables the muscles to secure the bladder and other pelvic organs more effectively. Kegel requires instruction and assistance from the doctor or physical therapist to ensure that the routines are executed properly.
Utilizing monitoring tools for biofeedback helps to ensure that the right muscles are being tightened for the ideal duration and intensity. Kegel exercise will result in improvement of your symptoms but not decrease the size of prolapse.
- Vaginal pessary: It is a ring usually made of plastic or rubber and this device will be inserted into the vagina that bladder in place. Although a pessary does not correct or cure the prolapse itself, the additional support it offers may aid with symptoms. Patients are advised how to clean and reinstall it on their own. Pessaries are frequently used by women in place of surgery when the risk of the procedure is high.
Surgical treatment
If non-surgical treatment fails to solve the symptoms, surgical treatment may be necessary to correct the prolapse.
- Anterior colporrhaphy or anterior vaginal repair: entails pulling the prolapsed bladder back into place with stitches and trimming off any extra vaginal tissue. If the vaginal tissues appear to be particularly thin, the doctor may decide to fortify them and provide support using a specific type of tissue graft.
- Hysterectomy: the surgical removal of the uterus is recommended if the anterior prolapsed is caused by prolapsed uterus. In addition to treating the injured pelvic floor muscles, ligaments, and other tissues.
- Uretheral suspension: The doctor may also suggest one of several treatments to support the urethra and lessen the incontinence symptoms. This is applicable if the anterior prolapse is accompanied by stress incontinence which causes urine to leak during physical activity or exertion.
- Obliterative surgery: treatment that narrows or seals off all or a portion of the vagina to give the bladder extra support. After this procedure, a woman can no longer engage in vaginal intercourse.
It is recommended to postpone surgery until after having children if you’re considering getting pregnant. As a temporary remedy, pessary or Kegel exercise may help ease the symptoms. The results of surgery can last for many years, but there is a chance that the prolapse will reoccur, necessitating another surgery.