Overview
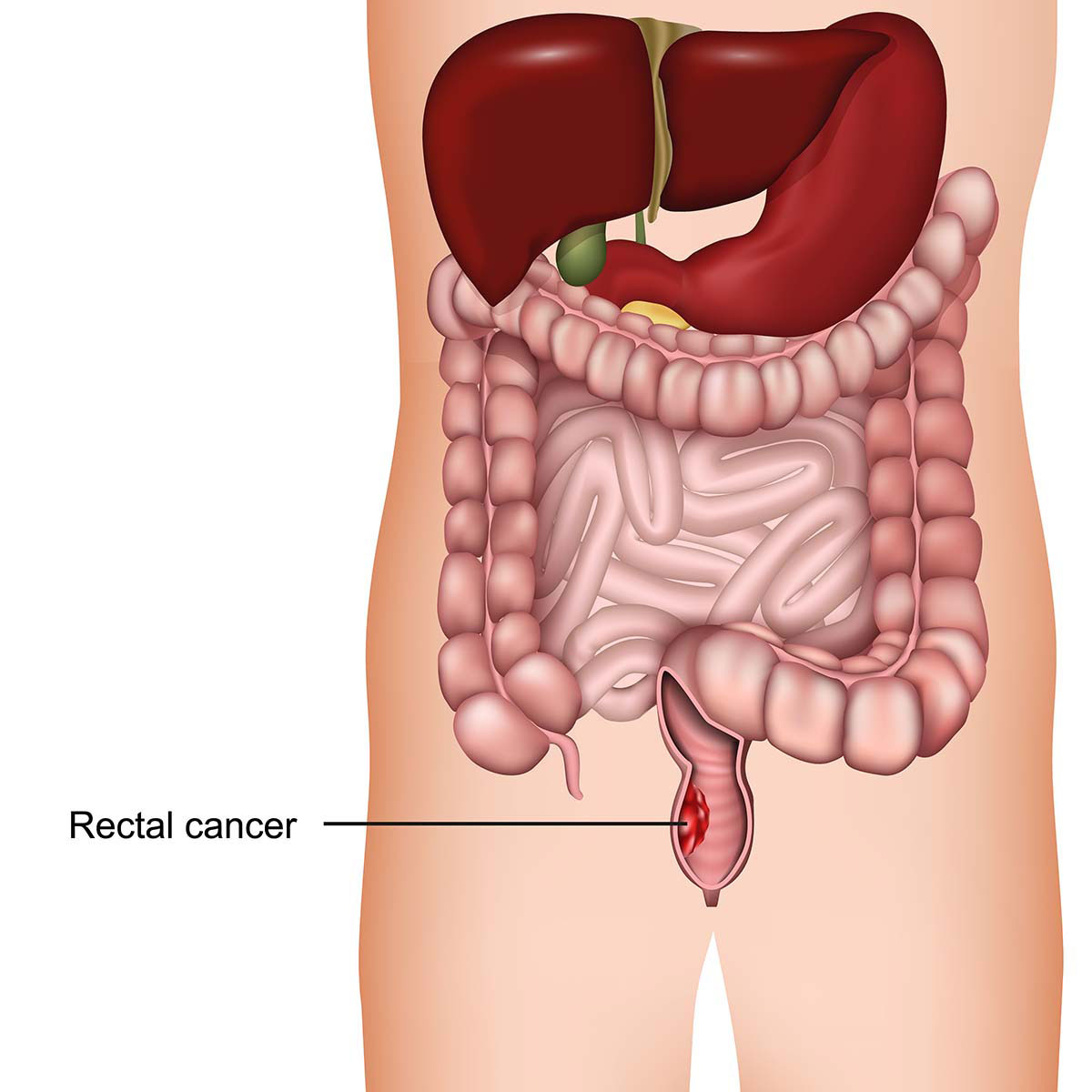
The rectum is the last part of the intestinal tract which starts from the end part of the colon down to the anus. Rectal cancer begins at the rectum. When cancer occurs inside the colon it is called colon cancer. When both rectal and colon cancer occur together, it is called “colorectal cancer”. Rectal and colon cancer may have a lot of similarities but they have different treatments. The reason is because the rectum is quite attached to the other organs which makes it difficult to surgically remove rectal cancer.
Symptoms
Rectal cancer may manifest with many signs and symptoms such as:
- Changes in bowel movement such as diarrhea or constipation or bowel movement that has become more frequent.
- Feeling of being unable to empty the large bowel
- Abdominal pain or cramping
- Maroon-colored or black-colored stool
- Narrow stool
- Rectal bleeding
- Unexplained weight loss
- Fatigue
If these symptoms persist, consult your doctor.
Causes
Rectal cancer starts when the DNA of the healthy cells mutate causing uncontrolled duplication, resulting in forming a mass of cells also known as a tumor. This tumor then starts to invade and destroy the healthy cell and could metastasize (spread to other parts of the body).
Inherited gene mutations that increase the risk of colon and rectal cancer
There are two common syndromes of colorectal abnormalities which relates to higher risk of developing colorectal cancer:
- Hereditary Nonpolyposis Colorectal Cancer (HNPCC) or Lynch syndrome. May have higher risk to acquire colon cancer and other types of cancers in people, even those who are less than 50 years old.
- Familial Adenomatous Polyposis (FAP). This is a rare condition which causes colon and rectum to have multiple polyps and has a higher chance of developing colon or rectal cancer before 40 years old.
If you have a family history of colorectal cancer, consult your doctor to perform proper genetic tests or other diagnostic tests.
Risk factors
Rectal and colon cancer may have the same risk factors such as.
- Age. Colorectal cancer may be acquired even before the age of 50 but most people with this cancer are older than 50 years old.
- African-American race. Being African-American has a higher risk of developing colorectal cancer.
- A personal history of colorectal cancer or polyps. Having a history of colon cancer, rectal cancer or adenomatous polyps.
- Inflammatory bowel disease. Having ulcerative colitis or Crohn’s disease which are chronic inflammatory diseases of the rectum and colon.
- Family history of colorectal cancer. People with a first-degree relative (parent, sibling, or child) with colon cancer increase the risk of developing colon cancer.
- Eating less vegetables. Eating diet low in vegetables could put patients at risk of developing colon cancer and rectal cancer. Certain studies have revealed that high consumption of red meat and processed meat could also be a contributing factor for colon cancer to occur.
- Inactive lifestyle. People living a sedentary lifestyle are likely to have colon cancer. Consistent physical activities may decrease the chance of developing the disease.
- Diabetes. Having a poorly managed type 2 diabetes.
- Radiation therapy for previous cancer. Radiation therapy applied to the abdomen for previous cancer treatment increases the chance of having colon cancer.
- Obesity. Being obese puts patients at risk of colon cancer
- Smoking. Smoking increases the risk of having colon cancer.
- Alcohol drinking. Heavy consumption of alcohol raises the risk of getting colon cancer
Diagnosis
Investigations for diagnosing rectal cancer
Screening tests to diagnose rectal cancer are as follows:
- Colonoscopy. A flexible tube with a camera is inserted into the rectum to the colon and inspects the structures inside. Colon examination on the affected area may be recommended if the doctor suspects cancer.
- Biopsy. During colonoscopy, the doctor will insert surgical instrument into the scope to take out tissue sample for examination under a microscope to examine the type of cancer cell, how aggressive the cancer is, which will know the prognosis of the disease and identify proper treatment.
Investigations for evaluating severity of rectal cancer
The next step after cancer diagnosis is to stage the cancer such as:
- Complete Blood Count (CBC). Checks for various types of blood cells. Also, if the red blood cells have significantly decreased (anemia), it may indicate blood loss due to the presence of a tumor. Increased white blood cells also indicate infection which is harmful when the tumor is on the rectal wall.
- Blood tests to measure organ function. High chemical levels in the blood may indicate that cancer has spread into the liver or kidney.
- Carcinoembryonic Antigen (CEA). CEA testing is particularly useful in monitoring your response to treatment. CEA is a tumor marker which may be increased in people with colorectal cancer.
- Computed Tomography (CT) scan of the chest. A diagnostic imaging test that investigates whether the cancer has spread to other organs of the body.
- Magnetic Resonance Imaging (MRI) of the pelvis. Shows more detailed images of the organs, muscles, lymph nodes and other tissues around the rectal tumor.
- Positron Emission Tomography (PET) scan. This procedure uses special dye with radioactive tracers (by ingestion, intravenously or inhalation) to view a more detailed structure of the affected area.
These tests will determine the stage of cancer which ranges from 0 (means the cancer is locally contained on the lining of the rectum only) to IV (means that the cancer is in its advanced stage and has spread to other parts of the body).
Treatment
A single or a combination of treatments may be suggested to manage and treat rectal cancer.
Surgery
The following surgical options are available to remove rectal cancer:
- Removing very small cancers from the inside of the rectum. Small sized rectal cancer may be removed using a colonoscope (trans-anal local excision).
- Removing all or part of the rectum. If the rectal cancer is quite far from the rectal canal, all parts of the rectum including nearby tissue and lymph nodes can be surgically removed (low anterior resection). This procedure does not remove the anus so the body can still eliminate waste normally. The technique is based on the affected area. If the upper part of the rectum is removed, the colon will be re-attached back to the rectum that is left over (colorectal anastomosis). If the lower portion of the rectum is removed, the colon will be formed like a pouch that can be joined to the anus (colo–anal anastomosis).
- Removing the rectum and anus. An Abdominoperineal Resection (APR) may be performed to remove the rectum, anus, nearby lymph nodes and some parts of the colon. This procedure is done if the cancer has reached near the anus, damaging the nerves that control bowel movement. An opening will be created in the abdomen and attach the colon that is left (colostomy). A colostomy bag will then be attached to the opening to collect waste materials from the colon.
Radiation therapy
The body is exposed to a high radiation to eradicate cancer cells.
Chemotherapy
Chemotherapy medications are taken orally or intravenously to kill cancer cells. It is an option for cancers that has metastasized (spread to other parts of the body) or unresponsive to hormone therapy.
Combined chemotherapy and radiation therapy
A combination of chemotherapy and radiation may be used to eliminate a larger rectal cancer or if it has a high chance of recurrence. It can be done before or after the surgery or as a primary treatment for advanced cancer to control cancer growth.
Immunotherapy
Uses the body’s own immune system to fight cancer. Immunotherapy blocks the proteins produced by the cancer cells to hide from the body’s disease fighting immune system.
Targeted drug therapy
Medications are used to focus only on specific abnormalities in the cancer cells. Targeted therapy inhibits the abnormalities and kills the cancer cells.




