Overview
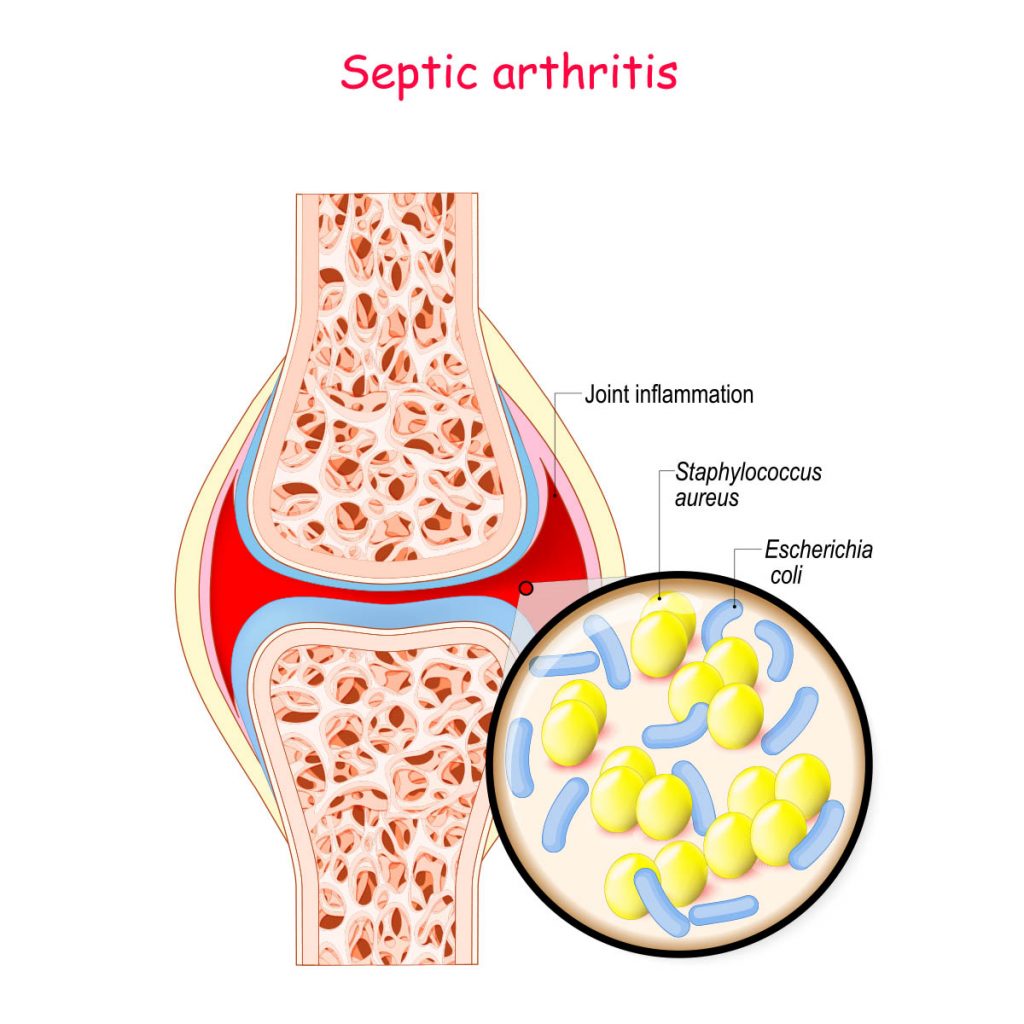
Septic arthritis (infectious arthritis) is an infection in the joint causing pain, swelling, redness and warmth. The infection can be triggered by germs from other parts of the body that spread to the joint through the bloodstream. This infection can also arise from a direct injury, such as animal bites or trauma that causes germs to be directly transferred into the joint.
Septic arthritis is more common in infants and adults. Patients with artificial joints have more chances to develop septic arthritis. The body parts that are mostly affected are knees, while the infection can also develop in hips, shoulders, and joints in other parts of the body. Cartilage and bone in the joint can be rapidly and severely damaged by the infection, therefore early treatment is extremely vital.
Treatment options include using a needle to drain the joint. This procedure can also be done during surgery. Antibiotics are generally required.
Septic Arthritis Symptoms in Adults
Patients often experience serious joint pain and difficulty moving the affected joint. The symptoms include swelling, redness, or warmness in the joints. Having a fever in addition to these symptoms is also a sign of septic arthritis, also called septic hip when it develops in the hip joint.
When septic arthritis develops in an artificial joint, the condition also known as prosthetic joint infection. In post knee or hip replacement surgery, symptoms like mild pain and swelling may arise several months or years after. Another sign includes loosening of the joint, which can be very painful when moving or putting pressure. The pain tends to be relieved after a rest. However, the joint could be dislocated if the condition is severe.
Consulting a doctor is vital if the patient has abrupt extreme joint pain.
Causes
Bacterial, viral, or fungal infections are the most common causes of septic arthritis and septic hip. The most common organism causing septic arthritis is Staphylococcus aureus (staph).
When an infection spreads to the bloodstream and enters the joint space, septic arthritis could develop. In rare cases, the infection would enter via punctured wound, injection, or surgical procedure in or around a joint, such as joint replacement surgery.
The environment of the joint has a mild protecting property that can protect itself from infection. As a result of infection, inflammation process in your body may develop, which may raise pressure and minimize blood flow within the joint. This further increases the damage.
Risk factors
- Previous joint problems or having chronic diseases that have impacts on the joints. Some of the diseases that may raise the risk of developing septic arthritis are osteoarthritis, gout, rheumatoid arthritis, or lupus. Undergoing joint surgery or having joint injury from the past may also increase the risk.
- Prosthesis joint from joint replacement surgery can cause bacteria to enter the A prosthetic joint can also be infected in the case that infection could spread to the joint by bloodstream.
- Intake of medications for rheumatoid arthritis has an increased risk of developing septic arthritis because the medicines could suppress the immune system, resulting in infection. Patients who have rheumatoid arthritis cannot be easily diagnosed with septic arthritis as the two conditions share common signs and symptoms.
- Fragile skin or skin that can be broken easily and has poor healing properties allows bacteria to enter the body. Psoriasis, eczema and infected wounds on the skin are risk factors of septic arthritis.
- Having weak immune system increases the risk of developing septic arthritis. Patients with diabetes, kidney, and liver diseases fall into this group. As well as those patients who are required to take medicines that suppress immune systems.
- Joint trauma involves direct injury that causes infection to penetrate into the joint directly, such as animal attacks or bites wounds, wounds that are punctured or cuts in the joint.
Patients with a combination of risk factors are at higher risk of developing septic arthritis than those who have a single risk factor.
Diagnosis
- Joint fluid analysis is a method of withdrawing fluid from the affected joint by inserting a needle and sending the joint fluid for a laboratory test, which can determine the organism that causes the infection. Doctor will prescribe the medication accordingly.
- Blood tests are carried out to rule out if there are any signs of bloodstream infection.
- Imaging tests such as X-rays of the affected joint to evaluate the damage or to see if there is a loosening of an artificial joint.
If suspected that you have prosthetic joint infection, a special scan that requires swallowing or injecting a tiny amount of radioactive chemical would be used.
Treatment
Doctors primarily uses joint drainage and antibiotics to treat patients with septic arthritis.
Joint drainage
Joint drainage is a removal of fluid from the infected joint. The followings are the drainage methods:
- Needle is inserted into the infected joint space to drain the fluid.
- Scope procedure is an arthroscopy, a procedure that is carried out by making a small incision to place a flexible tube with a video camera on the tip through to the joint space. Tubes for suctioning and draining are then inserted through cut around the joint.
- Open surgery is chosen for certain joints like hip joints that fluid cannot be drained with a needle or an arthroscopy.
Antibiotics
It is crucial for doctor to identify the organism behind the causing of the infection, so the right medication can be prescribed. Initially, antibiotics given through intravenous then it may be possible to change to oral antibiotics. Generally, the medication is taken for two to six weeks. Side effects of antibiotics are nausea, vomiting and diarrhea.
Removal of joint replacement
In case where artificial joint is infected, the condition will be treated by removing the joint and implanting a device composed of antibiotic cement to leave a space in the joint. Cases where a joint replacement cannot be done, the doctor will clean up the joint and trim excess tissues that have been destroyed and keep the artificial joint in its original place. Intravenous antibiotics will be given primarily then followed by oral antibiotics. The medications should be taken for several months to prevent new infections from arising.