
Testicular cancer
Overview
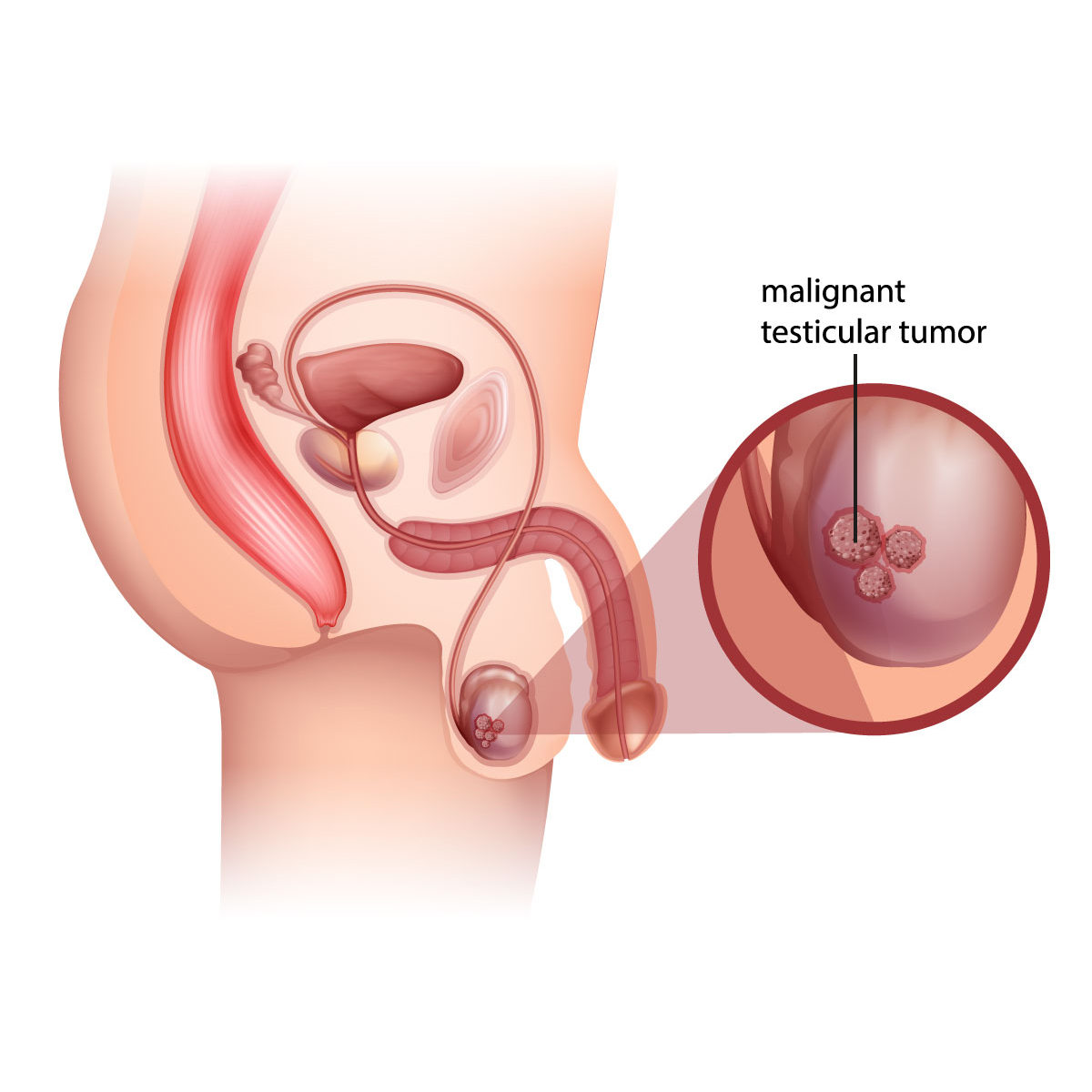
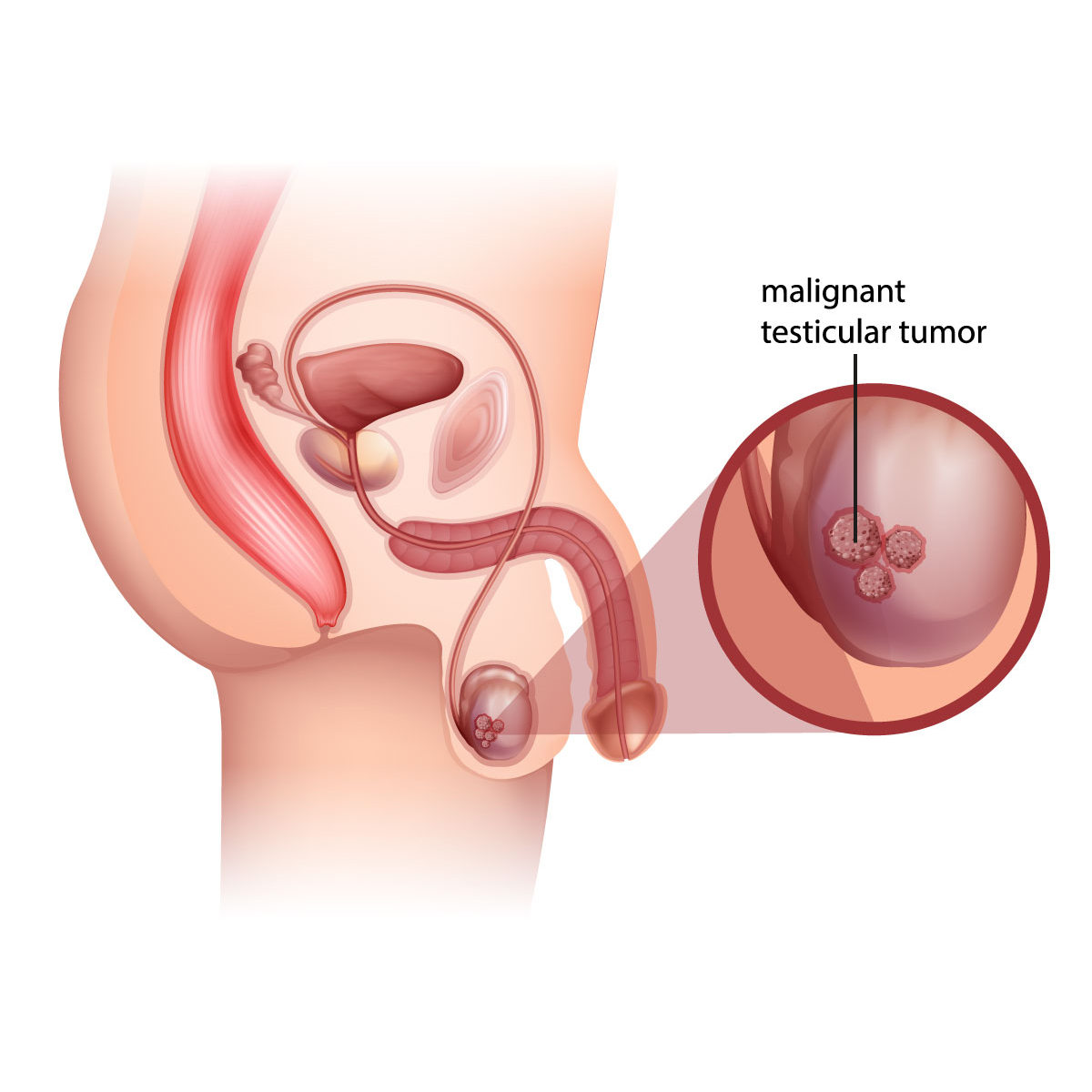
Testicular cancer is the development of cancer cell at either one or both testicles. Testicles are the two walnut-shaped glands that is located inside the scrotum (sac of skin under the penis), which produce male sex hormone and sperm. Testicular cancer is highly treatable even if the cancer has spread. Treatment for testicular cancer is based on the type and stage of the cancer.
Different types of testicular cancer
Most testicular cancers start in cells known as germ cells. These are the cells that develop into sperm.
There are two types of germs cells:
- Seminoma: These are more commonly in those that are of older age and tend to grow slower than non-seminoma.
- Non-seminoma. These grow rapidly and usually affect people in the late teen and early 30’s and are known to spread rapidly. The four types of non-seminoma tumors are named after its type of germ cell that they originate from. Non-seminoma tumors include embryonal carcinoma, yolk sac carcinoma, choriocarcinoma and teratoma.
Symptoms
Signs and symptoms of testicular cancer are as follows:
- Painless lump in the testicles
- Enlargement or swelling at either side of the testicles.
- Pain or discomfort at either the testicle or the scrotum
- Dull ache at the groin or abdomen
- Swelling or feeling of heaviness in the scrotum
If you notice any signs and symptoms that are persistent for more than two weeks, then you should make an appointment with your doctor.
Causes
In most cases the cause of testicular cancer is unknown how it could be from the multiplication of cancer cell that eventually developed into a tumor or a lump. The most common testicular cancer usually starts with the germ cells that formed into a tumor.
Risk factors
Factors that may increase testicular cancer risk includes:
- Age: it usually affects the late teens or men at early 30’s, however it could still affect male at all ages.
- Family History: it is highly possible to develop a testicular cancer if there is a history of cancer from the biological father or siblings.
- Undescended testicle: being born with undescended testicles (testicles fails to move from the abdomen to the scrotum before the birth) may increase the risk of having testicular cancer even it was surgically corrected.
- Race and ethnicity: testicular cancer are more common among white men.
Contact Information
service@vejthani.com






















