
Aortic valve regurgitation
Overview
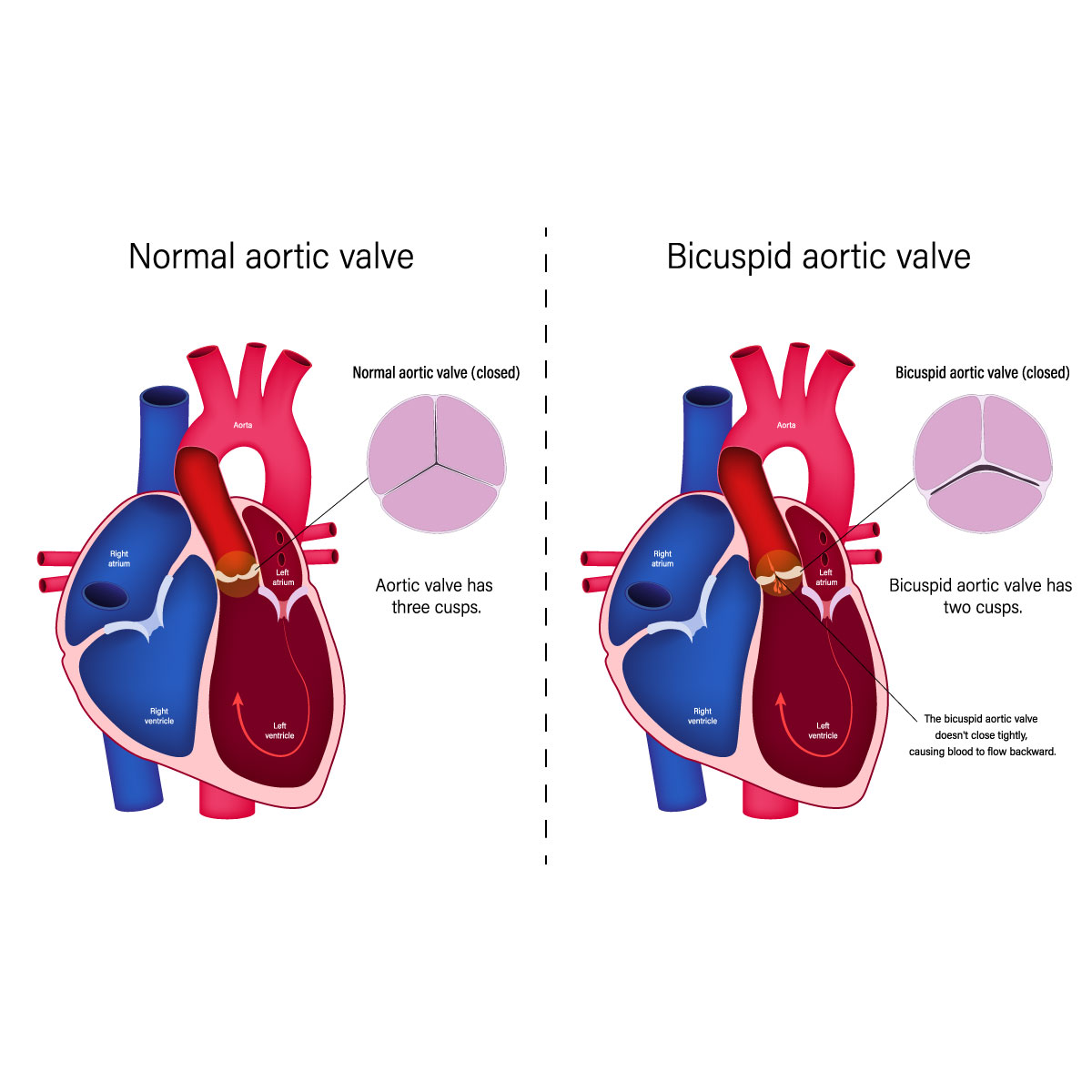
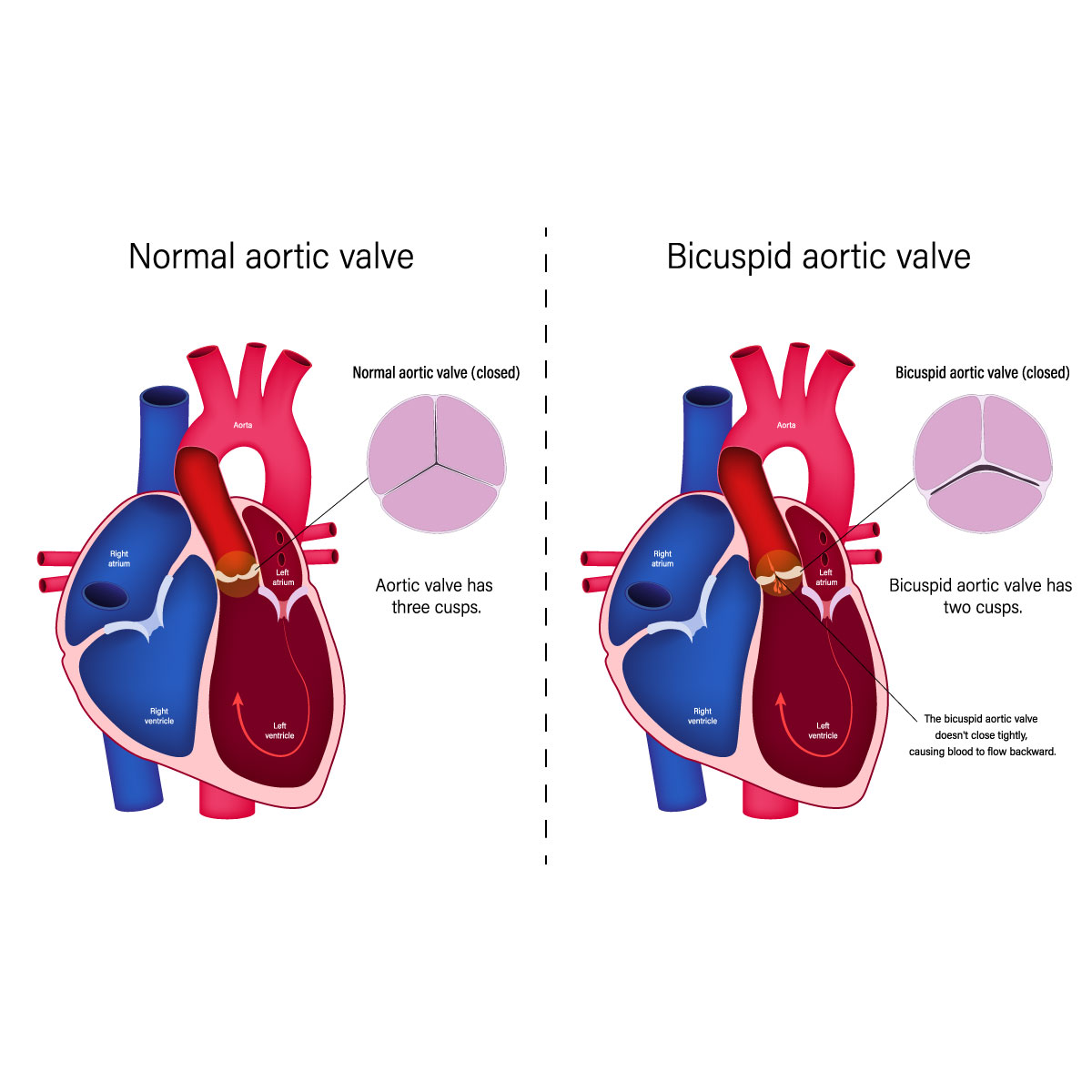
Aortic valve regurgitation, also known as aortic regurgitation, is a condition that develops when the leaflets known as cusps which open and close in a valve are not closed as tightly as they should, causing blood flow that is pumped out of the left ventricle (the main chamber of the heart) leak back into the chamber as a result of the disease. The leakage of aortic valve regurgitation prevents the heart from functioning properly by pumping blood to the rest of the body, which results in fatigue, or tiredness, or shortness of breath. This disease could suddenly develop, or it may take years to progress.
However, if it becomes severe surgical intervention is needed to repair or replace the aortic valve.
Symptoms
As aortic valve regurgitation is a slowly progressive disease, patients may be unaware of the disease as there may be no signs and symptoms. In some cases, the disease occurs suddenly due to a valve infection.
The signs and symptoms may include:
- Shortness of breath
- Chest pain, discomfort or tightness
- Fatigue
- Heart murmur
- Irregular pulse (arrhythmia)
- Lightheadedness or fainting
- Rapid heartbeat or palpitation
- Swelling of ankles and feet
If the patient is having any signs and symptoms, please consult the doctor.
Heart failure may occasionally be a factor in the development of aortic valve regurgitation. It is recommended to have a physical consultation with the specialist if the patient is experiencing tiredness that doesn’t improve with rest, shortness of breath, and swelling of ankles and feet, this may indicate heart failure.
Causes
One of the four valves that regulates blood flow through the heart is the aortic valve. It separates the major artery supplying your body with oxygen-rich blood (aorta) from the left ventricle, the heart’s primary pumping chamber. Each heartbeat causes the valve’s flaps (also known as cusps or leaflets) to open and close once. Aortic valve regurgitation develops when the blood flows regurgitate back into the left ventricle as a result of an abnormal closing of the aortic valve and it can lead to an enlargement of the heart chambers.
The larger left ventricle essentially exerts more force to keep a regular blood flow. Due to the disease the left ventricle and the heart eventually become weaker. Aortic valve regurgitation is a slow progressive disease (chronic) but it can induce instantly (acute) as a result of valve infection.
The following are some causes of aortic valve regurgitation:
- Congenital heart valve disease: These are at risk of experiencing aortic valve regurgitation at some point in their life because of these congenital heart defects. Rather than typical three distinct cusps valves, some people are born with aortic valves that have two cusps (bicuspid valve). In rare cases unicuspid and quadricuspid valves can occasionally exist.
A bicuspid valve increases the risk of developing one if they have a parent or sibling who has the disease. Even without a history of the disease in the family, someone can still have a bicuspid valve.
- Aortic stenosis (Narrowing of the aortic valve): this condition prevents the valve to open or close properly because of the blockage. This may be due to the calcium deposits that was build up that aortic valve stiffening and narrowing.
- Endocarditis: Inflammation of the lining of the heart’s chambers and valves. Infection is typically the cause of this life-threatening condition. The aortic valve may be damaged by it.
- Rheumatic fever: The damage to the heart valves might result from untreated strep throat infection. The aortic valve may develop scar tissue that will make the opening of the aortic valve become narrow, or it may become rough, allowing calcium deposits to build up. It’s called rheumatic heart disease.
- Other diseases: Marfan syndrome, a connective tissue disorder, and some autoimmune diseases such as lupus can cause the aorta and aortic valve to expand and cause regurgitation.
- Tear or injury at the aorta: blood may flow backward through the aortic valve as a result of a traumatic chest injury or an aortic tear (dissection).
Risk factors
The following are some risk factors that will likely develop into aortic valve regurgitation:
- Age: elderly is more like to be affected by the disease.
- Congenital heart disease: some certain heart conditions from birth could lead to aortic valve regurgitation.
- Previous infection: past illnesses such as rheumatic fever and infective endocarditis may have damaged the heart
- Other conditions: Marfan syndrome and aortic valve stenosis that can affect the heart.
- High blood pressure: patient who have high blood pressure have an increased risk of the developing aortic valve regurgitation.
Contact Information
service@vejthani.com






















