Imagine attending a party where you are supposed to enjoy but all of a sudden you found yourself taking trips to the restroom to void. It would not be that enjoyable anymore right? More so if you found out that you have peed on your underwear without you even noticing it.
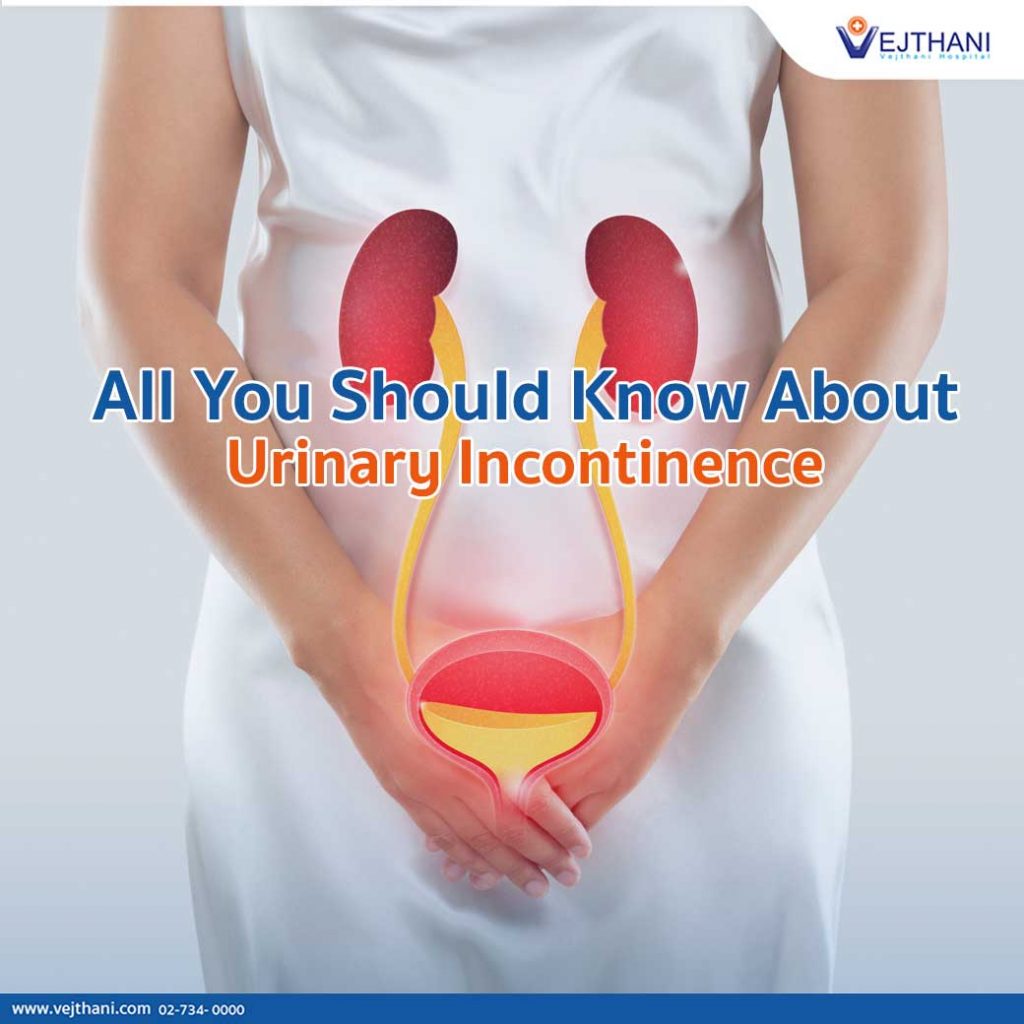
Millions of women experience involuntary loss of urine called urinary incontinence (UI). Some women may lose a few drops of urine while running or coughing. Others may feel a strong, sudden urge to urinate just before losing a large amount of urine. Many women experience both symptoms. UI can be slightly bothersome or totally debilitating. For some women, the risk of public embarrassment keeps them from enjoying many activities with their family and friends. Urine loss can also occur during sexual activity and cause tremendous emotional distress.
Women experience UI twice as often as men. Conditions which can lead to urinary incontinence include:
- Pregnancy and childbirth
- Menopausal
- Neurologic Injury
- Birth Defect
- Stroke
- Multiple Sclerosis
- Physical problems associated with Aging
Incontinence occurs because of problems with muscles and nerves that help to hold or release urine. The body stores urine—water and wastes removed by the kidneys—in the bladder, a balloon-like organ. The bladder connects to the urethra, the tube through which urine leaves the body.
During urination, muscles in the wall of the bladder contract, forcing urine out of the bladder and into the urethra. At the same time, sphincter muscles surrounding the urethra relax, letting urine pass out of the body. Incontinence will occur if your bladder muscles suddenly contract or the sphincter muscles are not strong enough to hold back urine. Urine may escape with less pressure than usual if the muscles are damaged, causing a change in the position of the bladder. Obesity, which is associated with increased abdominal pressure, can worsen incontinence. Fortunately, weight loss can reduce its severity.
| Types of Urinary Incontinence | |
| Stress | Leakage of small amounts of urine during physical movement (coughing, sneezing, exercising). |
| Urge | Leakage of large amounts of urine at unexpected times, including during sleep. |
| Overactive Bladder | Urinary frequency and urgency, with or without urge incontinence. |
| Functional | Untimely urination because of physical disability, external obstacles, or problems in thinking or communicating that prevents a person from reaching a toilet. |
| Overflow | Unexpected leakage of small amounts of urine because of a full bladder. |
| Mixed | Usually the occurrence of stress and urge incontinence together. |
| Transient | Leakage that occurs temporarily because of a situation that will pass (infection, taking a new medication, colds with coughing). |
How to Evaluate Urinary Incontinence
- Bladder stress test— coughing vigorously as the doctor watches for loss of urine from the urinary opening.
- Urinalysis and urine culture— laboratory technicians test your urine for evidence of infection, urinary stones, or other contributing causes.
- Ultrasound— uses sound waves to create an image of the kidneys, ureters, bladder, and urethra.
- Cystoscopy— the doctor inserts a thin tube with a tiny camera in the urethra to see inside the urethra and bladder.
- Urodynamics— various techniques measure pressure in the bladder and the flow of urine.
Treatment for Urinary Incontinence
Behavioral techniques
- Bladder training, to delay urination after you get the urge to go. You may start by trying to hold off for 10 minutes every time you feel an urge to urinate. The goal is to lengthen the time between trips to the toilet until you’re urinating only every two to four hours.
- Double voiding, learn to empty your bladder more completely to avoid overflow incontinence. Double voiding means urinating, then waiting a few minutes and trying again.
- Scheduled toilet trips, urinate every two to four hours rather than waiting for the need to go.
- Fluid and diet management, to regain control of your bladder. You may need to cut back on or avoid alcohol, caffeine or acidic foods. Reducing liquid consumption, losing weight or increasing physical activity also can ease the problem.
Pelvic floor muscle exercises
Do these exercises frequently to strengthen the muscles that help control urination. Also known as Kegel exercises, these techniques are especially effective for stress incontinence but may also help urge incontinence.
To do pelvic floor muscle exercises, imagine that you’re trying to stop your urine flow. Then:
- Tighten (contract) the muscles you would use to stop urinating and hold for five seconds, and then relax for five seconds. (If this is too difficult, start by holding for two seconds and relaxing for three seconds.)
- Work up to holding the contractions for 10 seconds at a time.
- Aim for at least three sets of 10 repetitions each day.
To help you identify and contract the right muscles, your doctor may suggest you work with a physical therapist or try biofeedback techniques.
Electrical stimulation
Electrodes are temporarily inserted into your rectum or vagina to stimulate and strengthen pelvic floor muscles. Gentle electrical stimulation can be effective for stress incontinence and urge incontinence, but you may need multiple treatments over several months.
Medications
Medications commonly used to treat incontinence include:
- Anticholinergics. These medications can calm an overactive bladder and may be helpful for urge incontinence. Examples include oxybutynin (Ditropan XL), tolterodine (Detrol), darifenacin (Enablex), fesoterodine (Toviaz), solifenacin (Vesicare) and trospium (Sanctura).
- Mirabegron (Myrbetriq). Used to treat urge incontinence, this medication relaxes the bladder muscle and can increase the amount of urine your bladder can hold. It may also increase the amount you are able to urinate at one time, helping to empty your bladder more completely.
- Alpha blockers. In men with urge or overflow incontinence, these medications relax bladder neck muscles and muscle fibers in the prostate and make it easier to empty the bladder. Examples include tamsulosin (Flomax), alfuzosin (Uroxatral), silodosin (Rapaflo), terazosin (Hytrin) and doxazosin (Cardura).
- Topical estrogen. Applying low-dose, topical estrogen in the form of a vaginal cream, ring or patch may help tone and rejuvenate tissues in the urethra and vaginal areas. This may reduce some of the symptoms of incontinence.
Note: Take medications as prescribed by physicians. Do not self-medicate
Medical devices
Devices designed to treat women with incontinence include:
- Urethral insert, a small, tampon-like disposable device inserted into the urethra before a specific activity, such as tennis, that can trigger incontinence. The insert acts as a plug to prevent leakage, and is removed before urination.
- Pessary, a stiff ring that you insert into your vagina and wear all day. The device helps hold up your bladder, which lies near the vagina, to prevent urine leakage. You may benefit from a pessary if you have incontinence due to a prolapsed bladder or uterus.
Interventional therapies
Interventional therapies that may help with incontinence include:
- Bulking material injections. A synthetic material is injected into tissue surrounding the urethra. The bulking material helps keep the urethra closed and reduce urine leakage. This procedure is generally much less effective than more-invasive treatments such as surgery for stress incontinence and usually needs to be repeated regularly.
- Botulinum toxin type A (Botox). Injections of Botox into the bladder muscle may benefit people who have an overactive bladder. Botox is generally prescribed to people only if other first line medications haven’t been successful.
- Nerve stimulators. A device resembling a pacemaker is implanted under your skin to deliver painless electrical pulses to the nerves involved in bladder control (sacral nerves). Stimulating the sacral nerves can control urge incontinence if other therapies haven’t worked. The device may be implanted under the skin in your buttock and connected directly to the sacral nerves or may deliver pulses to the sacral nerve via a nerve in the ankle.
Surgery
If other treatments aren’t working, several surgical procedures can treat the problems that cause urinary incontinence:
- Sling procedures. Strips of your body’s tissue, synthetic material or mesh are used to create a pelvic sling around your urethra and the area of thickened muscle where the bladder connects to the urethra (bladder neck). The sling helps keep the urethra closed, especially when you cough or sneeze. This procedure is used to treat stress incontinence.
- Bladder neck suspension. This procedure is designed to provide support to your urethra and bladder neck — an area of thickened muscle where the bladder connects to the urethra. It involves an abdominal incision, so it’s done during general or spinal anesthesia.
- Prolapse surgery. In women with mixed incontinence and pelvic organ prolapse, surgery may include a combination of a sling procedure and prolapse surgery.
Absorbent Pads and Catheters
If medical treatments can’t completely eliminate your incontinence, you can try products that help ease the discomfort and inconvenience of leaking urine:
- Pads and protective garments. Most products are no more bulky than normal underwear and can be easily worn under everyday clothing. Men who have problems with dribbles of urine can use a drip collector — a small pocket of absorbent padding that’s worn over the penis and held in place by close-fitting underwear.
- Catheter. If you’re incontinent because your bladder doesn’t empty properly, your doctor may recommend that you learn to insert a soft tube (catheter) into your urethra several times a day to drain your bladder. You’ll be instructed on how to clean these catheters for safe reuse.
The Women’s Health Center at Vejthani Hospital provides thorough medical consultation and treatment of Ob/Gyne’s diseases by highly skilled specialists. Moreover, we perform Ob/Gyn check-up, cancer and female reproductive organs check-up. Our experienced obstetricians and gynaecologists are ready to answer all your questions and help ease your concerns on any related health issues.
For more information, contact
Women’s Health Center, Vejthani Hospital
Call 02-7340000 or Ext. 3200,3204
English Hotline: (+66)8-522 38888
- Readers Rating
- Rated 5 stars
5 / 5 ( Reviewers) - Spectacular
- Your Rating