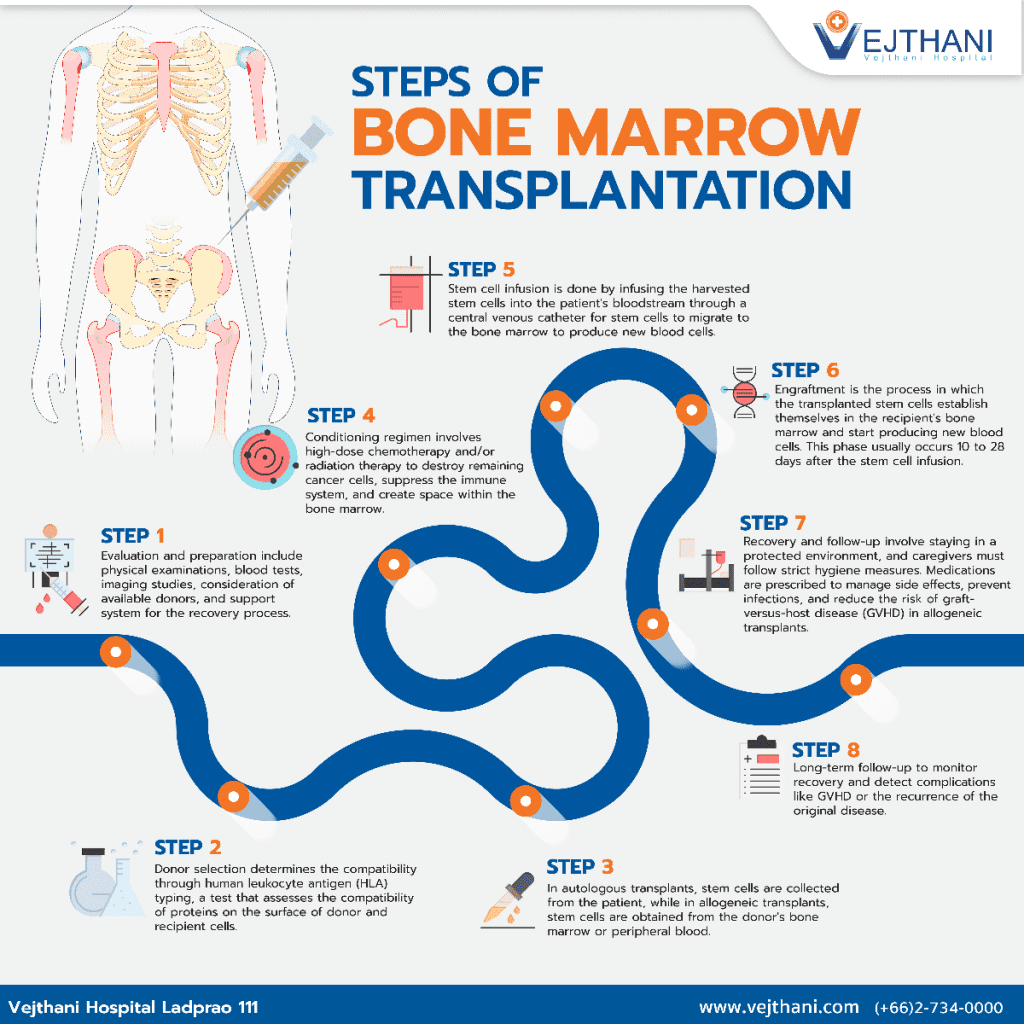
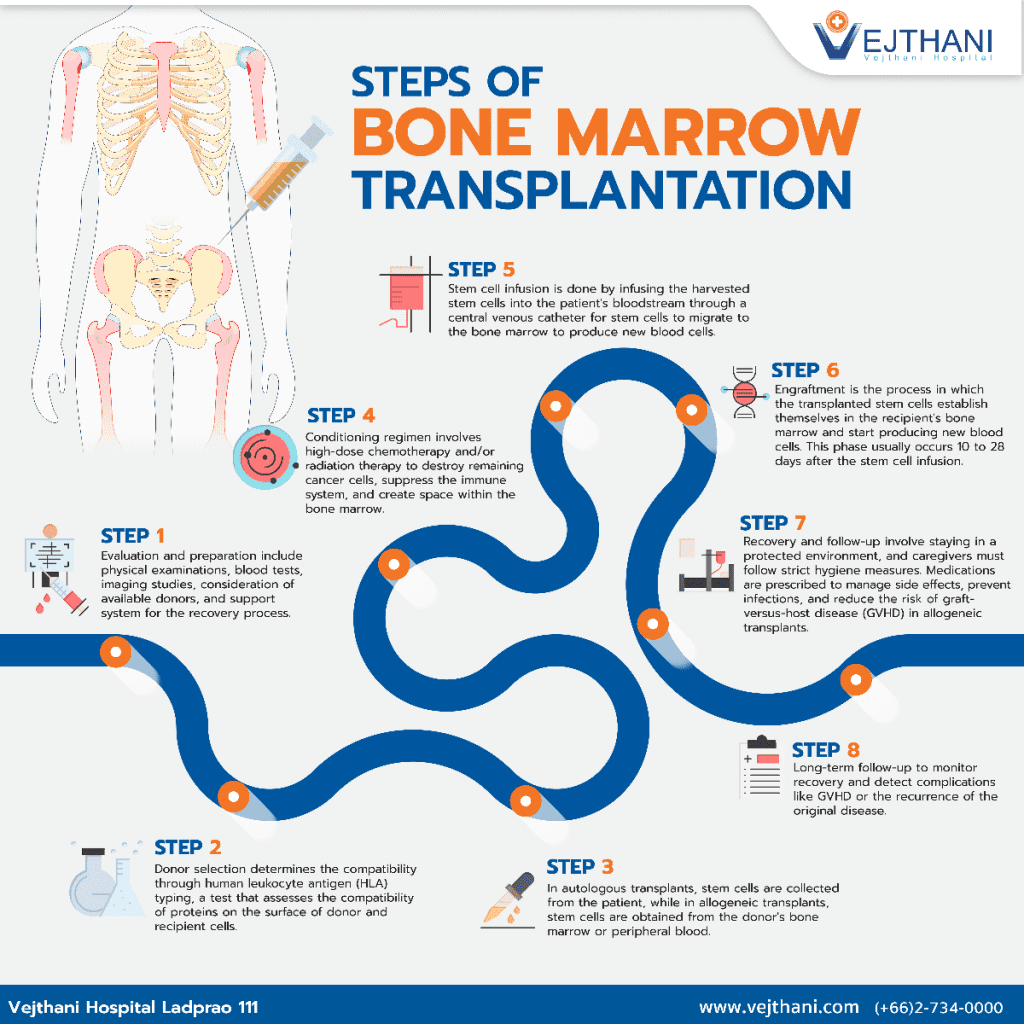
Bone marrow transplantation (BMT), also known as hematopoietic stem cell transplantation (HSCT), is a complex medical procedure involving several critical steps. The process can be broken down into the following stages:
- Evaluation and preparation: Before BMT, patients undergo a thorough evaluation to determine their eligibility for the procedure. This assessment includes physical examinations, blood tests, and imaging studies to assess overall health and disease status. The healthcare team also considers factors such as the availability of a suitable donor and the patient’s support system during the recovery process.
- Donor selection: A compatible donor is essential for the success of BMT. In autologous transplants, patients serve as their own donors, while allogeneic transplants require stem cells from a related or unrelated donor. Donor compatibility is determined through human leukocyte antigen (HLA) typing, a test that assesses the compatibility of proteins on the surface of donor and recipient cells.
- Stem cell collection: Once a suitable donor is identified, the process of stem cell collection, or harvesting, begins. In autologous transplants, stem cells are collected from the patient, usually after administering growth factors to stimulate stem cell production. In allogeneic transplants, stem cells are obtained from the donor’s bone marrow or peripheral blood, depending on the specific transplantation method.
- Conditioning regimen: Prior to stem cell infusion, patients undergo a conditioning regimen, which involves high-dose chemotherapy and/or radiation therapy. This process aims to destroy any remaining cancer cells, suppress the immune system to reduce the risk of rejection, and create space within the bone marrow for the new stem cells to grow.
- Stem cell infusion: After the conditioning regimen, the harvested stem cells are infused into the patient’s bloodstream through a central venous catheter. The procedure is similar to a blood transfusion and typically takes a few hours. The stem cells then migrate to the bone marrow, where they begin to produce new blood cells.
- Engraftment: Engraftment is the process through which the transplanted stem cells establish themselves in the recipient’s bone marrow and start producing new blood cells. This critical phase usually occurs within 10 to 28 days following the stem cell infusion. During this period, patients are closely monitored for signs of engraftment, such as rising blood cell counts.
- Recovery and follow-up: The recovery period after BMT can be lengthy and challenging. Patients are susceptible to infections and complications due to their weakened immune systems. Therefore, they are typically kept in a protected environment, and caregivers must follow strict hygiene measures. Medications are prescribed to manage side effects, prevent infections, and reduce the risk of graft-versus-host disease (GVHD) in allogeneic transplants.
- Long-term follow-up: After discharge from the hospital, patients continue to receive regular follow-up care to monitor their recovery and assess any late complications, such as GVHD or the recurrence of the original disease. This long-term follow-up may last for several years or even a lifetime, depending on the patient’s condition.
Bone marrow transplantation is a complex, multi-step process that requires careful planning and coordination among the patient, healthcare team, and donor. While BMT can be a life-saving treatment for various conditions, it carries inherent risks and demands a long recovery period, making thorough evaluation and follow-up crucial for success.
- Readers Rating
- Rated 4.9 stars
4.9 / 5 ( Reviewers) - Spectacular
- Your Rating