Overview
Trigeminal neuralgia, also referred to as tic douloureux, is a condition characterized by excruciating pain on one side of the face, resembling an electric shock. This chronic pain condition affects the trigeminal nerve, responsible for transmitting sensory information from the face to the brain. Even minor facial stimuli, like brushing teeth or applying makeup, can trigger intense agony in individuals suffering from trigeminal neuralgia. At first, you can encounter brief, mild attacks. However, trigeminal neuralgia can progress and result in longer, more frequent episodes of excruciating pain. Women experience trigeminal neuralgia more frequently than men do, and persons older than 50 are more prone to develop it.
Trigeminal neuralgia frequently affects only one side of the face unilaterally. If it’s bilateral, both sides will be impacted, but not simultaneously. Additionally, bilateral trigeminal neuralgia is very uncommon. It’s interesting to note that this condition typically affects the right side of the face more than the left.
Trigeminal neuralgia is a condition that offers various treatment options, indicating that individuals affected by it are not inevitably condemned to a lifetime of pain. Trigeminal neuralgia is typically successfully treated by doctors using drugs, injections, or surgery.
Types of trigeminal neuralgia
- Typical trigeminal neuralgia (Type 1). Sharp, acute, intermittent pain episodes are probably what you’ll encounter. From a few seconds to two minutes, you can experience pain and/or a burning feeling all over your face. There will be pain–free intervals between attacks, but this can go on for as long as two hours.
- Atypical trigeminal neuralgia (Type 2). This type is less severe and intense, but more ubiquitous. Along with continuous aches and pains, you’ll probably have constant agony, particularly stabbing and/or burning feelings. The symptoms of atypical trigeminal neuralgia could be more challenging to manage.
Symptoms
Trigeminal neuralgia can manifest with one or more of the following symptom patterns:
- Periodic episodes of excruciating, shooting, or stabbing pain that may seem electric shock–like
- Aches and pains brought on by facial spasms
- Periods of no discomfort for some people during multiple attacks that continue for days, weeks, months, or longer.
- Aches in the face, jaw, teeth, gums, or lips that are supplied by the trigeminal nerve, or less frequently in the eye and forehead
- Pain that comes on suddenly or that is brought on by actions like touching the face, chewing, speaking, or brushing teeth.
- Pain attacks can last anywhere between a few seconds and several minutes.
- Pain is infrequently experienced while resting at night
- Increasingly frequent and severe attacks over time
- Unilateral facial pain, impacting only one side at a time
- The pain can be localized to a specific area or radiate in a broader pattern.
Aside from the pain, there may be other symptoms as well.
It is advisable to seek medical attention if you experience facial pain, particularly if the pain is severe, recurring, or unresponsive to over–the–counter pain relievers. Consulting with a doctor is recommended in such cases.
Causes
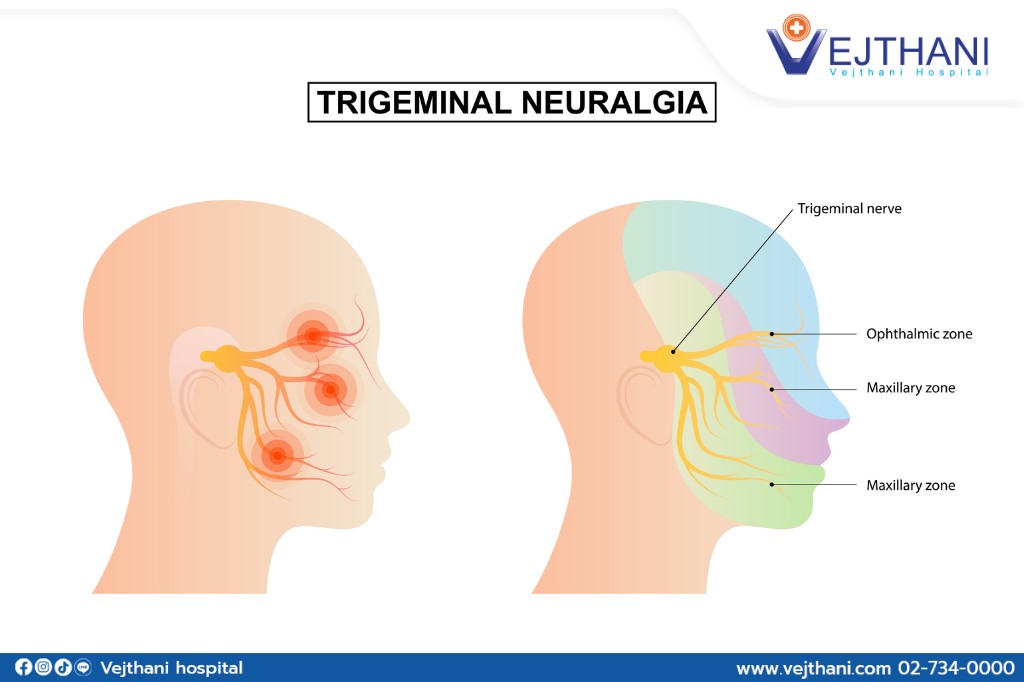
The trigeminal nerve’s normal function is interfered within trigeminal neuralgia. Typically, the issue is contact between the trigeminal nerve at the base of your brain and a typical blood vessel, in this case an artery or a vein. The nerve becomes malfunction as a result of the pressure this contact puts on it.
While one of the most frequent causes of trigeminal neuralgia is compression by a blood vessel, there are numerous other possible reasons as well. Some of them could be caused by multiple sclerosis or another condition that damages the myelin sheath that shields some nerves. A tumor pressing against the trigeminal nerve might also result in trigeminal neuralgia.
Trigeminal neuralgia may be brought on by a brain tumor or another abnormality in certain persons. Trigeminal neuralgia may also result from facial trauma, stroke, or surgical damages.
Triggers
Trigeminal neuralgia can be brought on by a number of factors, including:
- Talking
- Facial movement such as smiling
- Drinking
- Consuming food
- Brushing your teeth
- Washing or touching your face
- Shaving
- Applying makeup
- Wind blowing on your face
Diagnosis
Trigeminal neuralgia will be diagnosed by your doctor primarily based on how you describe the pain, which may include:
- Type. Trigeminal neuralgia–related pain occurs suddenly, shock–like and for a short period of time.
- Location. Your doctor will be able to determine whether the trigeminal nerve is implicated by checking at the areas of your face that are painful.
- Triggers. Normal triggers for pain associated with trigeminal neuralgia include eating, speaking, lightly touching your face, and even feeling a chilly wind.
To identify the underlying reasons of your disease and diagnose trigeminal neuralgia, your doctor may perform a variety of tests, including:
- Neurological assessment. Your healthcare provider has the expertise to identify the precise location of your pain and assess the potential involvement of trigeminal nerve branches if trigeminal neuralgia is suspected. They may perform a physical examination by touching and examining different areas of your face. Additionally, reflex testing can help your doctor determine whether your symptoms are caused by another condition or a compressed nerve. By conducting these assessments, your doctor can provide a more accurate diagnosis and guide you towards appropriate treatment options.
- Magnetic Resonance Imaging (MRI). To identify whether multiple sclerosis or a tumor is causing trigeminal neuralgia, your doctor might request an MRI of your head. When viewing the arteries and veins and highlighting blood flow, your doctor may occasionally inject a dye into a blood vessel.
An accurate diagnosis is essential as there are several medical conditions that can potentially cause facial pain. In order to rule out other possible causes, your doctor may recommend additional tests. These tests can help to eliminate other conditions and narrow down the underlying cause of your facial pain.
Treatment
Medication is commonly the initial treatment approach for trigeminal neuralgia, although some patients may not require it. However, some sufferers with the illness may eventually cease responding to treatment or have unfavorable side effects. Injections or surgery are additional trigeminal neuralgia treatments available for those patients.
Your doctor will treat the underlying problem if it’s determined that your condition is brought on by another factor, such as multiple sclerosis.
Medications
Your doctor will typically prescribe drugs to decrease or block the pain signals transmitted to your brain in order to treat trigeminal neuralgia.
- Anticonvulsants. Trigeminal neuralgia is commonly treated with carbamazepine, which has been proven to be successful in this regard. Oxcarbazepine, lamotrigine, valproate, and phenytoin are further anticonvulsant medications that could be utilized to treat trigeminal neuralgia. Various other medications, such as clonazepam, topiramate, pregabalin, and gabapentin, may also be utilized.
Your doctor might change the type of anticonvulsant you’re taking or up the dosage if it starts to lose its efficacy. Anticonvulsant side effects can include nausea, disorientation, drowsiness, and vertigo. Before beginning carbamazepine treatment, genetic testing may be advised since carbamazepine can cause a significant medication reaction in some persons, primarily those of Asian heritage.
- Antispasmodic agents. It is possible to take carbamazepine alone or in combination with muscle relaxants like baclofen. Drowsiness, nausea, and confusion are possible side effects.
- Botox injections. Small trials have suggested that onabotulinumtoxinA (Botox) injections could potentially provide relief from trigeminal neuralgia pain in individuals who no longer find relief from medication. However, further research is necessary before this treatment approach can be widely adopted for this condition.
Surgery
Trigeminal neuralgia surgery possibilities include:
- Microvascular decompression. To prevent the trigeminal root from malfunctioning, this technique includes shifting blood vessels or eliminating blood veins that are in contact with it. Your doctor creates an incision behind the ear on the side of your pain to perform microvascular decompression. Your surgeon will next insert a soft cushion between the trigeminal nerve and any arteries that are in direct touch with the nerve through a tiny hole in your skull.
Your surgeon might cut off the vein if it is pushing on the nerve. If no arteries are pushing on the trigeminal nerve, doctors may perform a neurectomy during this treatment.
Microvascular decompression can successfully lessen or eliminate pain for many years, however three out of ten persons will experience a recurrence of their pain within ten years. Reduced hearing, facial numbness or weakness, a stroke, or other problems are some of the dangers associated with microvascular decompression. The majority of patients do not experience face numbness following this surgery.
- Brain stereotactic radiosurgery (Gamma knife). The trigeminal nerve root is targeted with radiation during this treatment by a surgeon. Radiation is used in this operation to destroy the trigeminal nerve and lessen or remove pain. The onset of relief is slow and could last up to a month.
For the majority of patients, brain stereotactic radiosurgery is successful in removing pain. However, there is a chance of recurrence, typically within 3 to 5 years, as with all treatments. The procedure can be repeated if the pain reappears, or a different technique might be carried out. Common adverse effects include facial numbness, which might appear months or years after the operation.
Various treatment options, including rhizotomy, can be utilized to manage trigeminal neuralgia. Rhizotomy involves a surgical procedure which destroys nerve fibers to alleviate pain. Different types of rhizotomy techniques include:
- Glycerol injection. Your doctor will pass a needle through your face and into the base of your skull during this treatment. The trigeminal cistern, a little sac of spinal fluid that houses the trigeminal nerve ganglion, which is where the trigeminal nerve splits into three branches, and a portion of its root, is where your doctor inserts the needle. The trigeminal nerve is damaged and pain signals are blocked by a little injection of sterile glycerol, which is administered by your doctor.
Pain is frequently reduced by this process. However, many suffer from facial numbness or tingling, and some persons report a subsequent recurrence of pain.
- Balloon compression. During the procedure known as balloon compression, your doctor will insert a hollow needle through your face, guiding it to the passage of the trigeminal nerve at the base of your skull. Through this needle, a catheter equipped with a balloon is threaded by your doctor. The balloon is then inflated to a level that intentionally damages the trigeminal nerve, disrupting pain signals. Balloon compression has shown success in providing temporary relief for many patients in managing their discomfort. However, it’s important to note that most patients will experience some degree of temporary facial numbness following this procedure.
- Radiofrequency thermal lesioning. During the treatment known as radiofrequency thermal lesioning, the nerve fibers responsible for pain are selectively destroyed. Under anesthesia, your surgeon will insert a hollow needle through your face, directing it towards the trigeminal nerve as it passes through a skull base opening. At a certain point, you will be momentarily awakened from sedation by your doctor. An electrode is placed into the needle, and a weak electrical current is passed through its tip. You will be asked to indicate the location and timing of any tingling sensation you experience. Once your neurosurgeon identifies the specific area of the nerve causing your pain, you will be placed back under sedation. The electrode is then heated, creating a lesion or injury to the nerve fibers. Additional lesions may be made if your pain persists. Following radiofrequency thermal lesioning, it is common to experience temporary facial numbness. However, it’s important to note that after three to four years, pain can potentially return.




