Overview
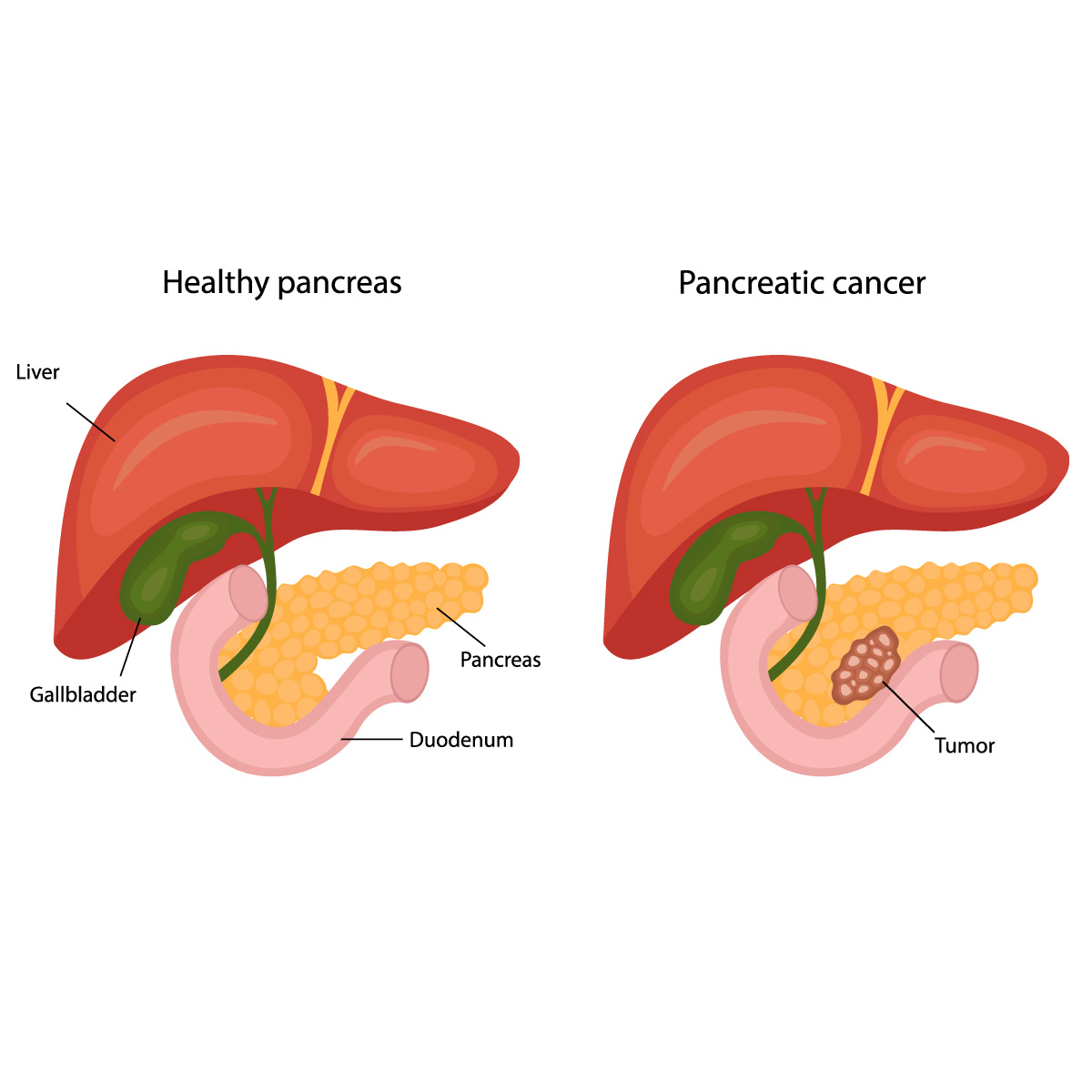
The pancreas is a pear-shaped organ that is approximately six inches long located behind the stomach. Its function is secreting hormones such as insulin to aid digestion and blood sugar regulation.
The mutation of pancreatic cell causes uncontrolled duplication resulting in forming a mass of cells also known as a pancreatic tumor. This tumor then begins to invade and destroy the healthy tissues. Untreated pancreatic cancer has the ability to spread to organs around it or to other parts of the body (metastasis).
Symptoms
There are usually no signs and symptoms seen in pancreatic cancer until the disease has become advanced. But if there are any, the following may be observed:
- Loss of appetite or unexplained weight loss
- Nausea and vomiting
- Abdominal pain radiating to the back
- Jaundice (yellowish discoloration of the skin and the sclera of the eyes)
- Light-colored stool
- Dark-colored urine
- New onset of diabetes
- Itchy skin
- Blood clots in the body
- Tiredness
If you notice these symptoms and it worries you, consult a doctor for proper diagnosis and treatment.
Risk factors
The following are the risk factors which may result in pancreatic cancer:
- Familial genetic disease that carries BRCA2 genetic mutation, Lynch syndrome and familial atypical mole-malignant melanoma (FAMMM) syndrome
- Pancreatic cancer in family
- Ashkenazi Jewish descent
- Race: African-American
- Gender: Male
- Old age (more than 65 year old)
- Having diabetes
- Having chronic pancreatitis (inflammation of the pancreas)
- Smoking
- Being obese or overweight
Diagnosis
The following tests may be recommended if the doctor suspects that the patient has pancreatic cancer:
- Imaging tests. Diagnostic tests visualize the images of the internal organ. The tests used to diagnose pancreatic cancer are ultrasound, Computerized Tomography (CT) scan, Magnetic Resonance Imaging (MRI) and Positron Emission Tomography (PET) scan.
- Endoscopy. The pancreas may be viewed inside the digestive system using an Endoscopic Ultrasound (EUS). An investigation consisting of a flexible thin tube connected to a tiny camera, which will be inserted into a patient’s mouth passing through the esophagus and stomach, and into the duodenum to look at the pancreas and get its images.
- Biopsy. This is a process of taking a sample of body tissue for examination under a microscope to check for cancer which is commonly done during EUS by inserting the instrument inside the endoscope. Another way is puncturing your skin where the pancreas is located with a small needle and taking a small sample (fine-needle aspiration).
- Blood test. These are blood tests in order to check if there is an over production of carbohydrate antigen (CA) 19-9 which a protein that is produced by the pancreatic cancer cells.
After pancreatic cancer diagnosis, the doctor will stage the cancer to determine the cancer extent. This determines which treatment is intended for the pancreatic cancer stage.
Staging ranges from 0 to IV The lowest stage means that the cancer is located in the pancreas and stage IV means that the cancer has already spread into other parts of the body.
Treatment
The stage and location of the cancer will determine its treatment. The purpose of treatment is to kill the pancreatic cancer but if this option is not possible, quality of life improvement and avoiding further cancer spread or growth is the goal.
-
Surgery
- Whipple procedure (pancreaticoduodenectomy). The Whipple procedure is an operation which will remove the head of the pancreas, the duodenum (the first part of small intestine), the gallbladder and portions of the bile duct. Some portions of the stomach and colon may also be removed in some cases. The remaining parts will be reconnected to allow food digestion.
- Distal pancreatectomy. Surgically removes tumor in the body and tail (left side) of the pancreas. It may also include the removal of the spleen.
- Total pancreatectomy. Removes the whole pancreas if it has been fully affected with cancer. If the pancreas has been totally removed, patient also requires lifelong insulin and pancreatic enzyme replacement.
- Removal of tumors affecting nearby blood vessels. Highly specialized surgeons are needed in order to perform the removal or reconstruction of affected nearby blood vessels with tumor. At this stage that the cancer is already in advance stage, Whipple procedure or other pancreatic surgeries may no longer effective.
Chemotherapy
Chemotherapy medications are administered orally or intravenously in order to kill pancreatic cancer cells. It may also be combined with radiation therapy (chemoradiation) if the cancer has not spread (metastasized) to other parts of the body. Chemoradiation may be done before surgery to decrease the size of the tumor and enables it to be surgically removed. It may also be used after surgery to ensure that there are no cancer cells left and avoid recurrence. In stage IV cancer, chemotherapy may be used to control cancer growth and prolong life.
Radiation therapy
This treatment uses high power beams such as X-rays and protons or by the placement of radioactive material inside the body nearby the cancerous area in order to kill the cells. It may be done before or after surgery or in combination with chemotherapy.
Targeted therapy
Targets genes or proteins that assists with the growth of cancer. This treatment option is determined by performing genetic testing
Immunotherapy
Assists the body’s immunity to counteract cancer. Although the success rate of immunotherapy is only 1% of the genetic cancer population.




