Overview
Heart arrhythmia is an abnormal heart rate or rhythm due to abnormalities in electrical signals. This disease causes the heart to beat irregularly, too fast (tachycardia) or too slow (bradycardia).
Heart arrhythmia can often be harmless, but some can turn into a serious heart condition. Heart arrhythmia can be treated by stabilizing the heart rhythm with medications, catheter surgery, implanted devices, as well as lifestyle adjustment for preventive measures.
Types
The types of heart arrhythmia based on the heart rate, as follows:
- Tachycardia: is a fast resting heart rate of over 100 beats per minute.
- Bradycardia: is a slow heartbeat with a rate below 60 beats per minute.
Tachycardia
Tachycardia is an abnormally rapid heartbeat of more than 100 beats per minutes. There are different types of tachycardia including:
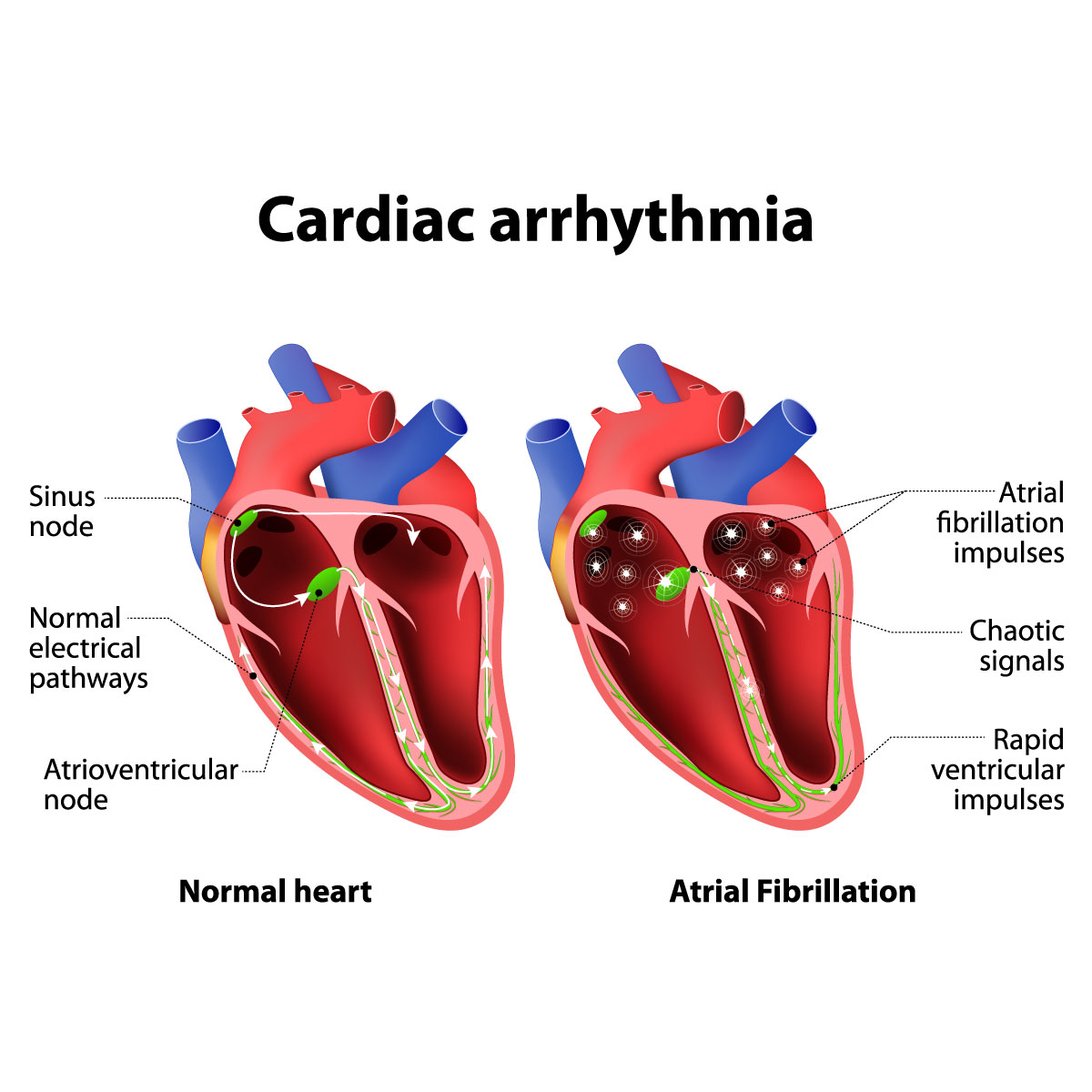
- Atrial fibrillation: It causes a fast and uncoordinated heart rate, which may resolve on its own or require treatment. In severe circumstances, this disease may lead to stroke.
- Atrial flutter: Its symptoms are similar to atrial fibrillation, including the risk of stroke. However, atrial flutter causes less chaotic heartbeats.
- Supraventricular tachycardia: is a rapid heart rate that begins and end abruptly. These abnormal rhythms originate from above the lower heart chambers.
- Ventricular fibrillation: is an abnormal electrical signal that start from the lower chambers and causes rapid irregular heartbeat. During ventricular fibrillation, the heart does not pump blood to the rest of the body. This is an emergency that requires immediate medical attention.
Certain major heart conditions or serious injury are associated with the development of ventricular fibrillation. - Ventricular tachycardia: is an abnormal electrical signal that starts from the lower chamber and causes rapid regular heartbeat. The rapid heartbeat does not allow the ventricle to fill up blood before pumping the blood out to the rest of the body.This type of arrhythmia can be fatal and requires immediate treatment, especially among people with heart disease.
Bradycardia
Bradycardia is a condition that the heart beats lower than 60 beats per minutes. However, healthy people can have a heart rate under 60 beats without any problems. There are different types of bradycardia including:
- Sick sinus syndrome (sinus node dysfunction): The sinus node function as the natural pacemaker that control the heartbeat. Sick sinus syndrome is a disease that affects the sinus node. It might alternately cause bradycardia and tachycardia. It occurs commonly in older adults.
- Conduction block: This type of arrhythmia cause blockage in electrical pathways of the heart, slowing down or even stopping your heartbeats. This cardiac blockage condition can be either asymptomatic or symptomatic. The symptoms that can be found include skipped beats and bradycardia.
Premature heartbeats
Premature heartbeats generally occur one at a time, which alternates with occasional normal beating. This heart condition might be caused by either premature atrial or ventricular contractions, where extra beats originate in the top chamber and the bottom chamber of the heart, respectively. The causes of premature heartbeats are stress, excessive exercise and too much consumption of stimulants such as caffeine or nicotine.
Although premature heartbeats can cause symptoms like skipped heartbeats, the disease is not severe and has no serious complications.
However, those with heart disease are at a greater risk of developing persistent arrhythmia even when resting, which causes premature beats to frequently occur for many years, finally leading to the weakening of the heart.
Symptoms
As heart arrhythmia can be asymptomatic, the disease might sometimes be accidentally found during a general health checkup.
Common signs and symptoms of arrhythmias include:
- Palpitations
- Fast heartbeat, or tachycardia
- Slow heartbeat, or bradycardia
- Chest tightness
- Difficulty in breathing
Less common symptoms of the disease include:
- Stress
- Tiredness
- Dizziness
- Sweating
- Fainting or passing out
If you have any of these symptoms, seek emergency medical care immediately:
- Difficulty in breathing
- Dizziness
- Fainting or passing out
- Chest pain
You are still recommended to see a doctor even though you have less severe symptoms like irregular heartbeats, either too slow or too fast, or having skipped heartbeats.
Ventricular fibrillation, which is a form of arrhythmia, can make the blood pressure quickly drop, causing fainting within a matter of seconds, as well as making the breathing and the heart’s beating stop. You are recommended to follow the following steps if you find a patient experiencing any of the symptoms:
- Call the police or an ambulance as soon as possible.
- If there is no one trained in cardiopulmonary resuscitation (CPR) nearby, do hands-only CPR. You are supposed to push quickly and strongly on the chest area for 100-120 times per minute while waiting for the ambulance to arrive. Be noted that there is no need to do rescue breathing.
- If you or someone nearby trained in CPR, do CPR while waiting for an electrical shock (defibrillation). CPR makes blood flow to organs more easily.
- Use a portable defibrillation device called automated external defibrillator (AED). This tool sends a shock that can make the heart that has stopped beating beat again. AED is easy and safe to be used by untrained people as it sends a shock only when necessary.
Causes
The heart consist out of four chambers, two upper chambers called the atria and two lower chambers called the ventricles. The sinus node in the upper right chamber, or the atrium, acts as a natural pacemaker which controls the heart beats by sending electrical signals. When the atria receive these signals, the heart muscles start to contract and pump blood into the ventricles. The heart signals will continue to go down to the AV node, where they slow down to allow blood to fill the ventricles. After that, the ventricles will contract to pump blood to the lungs or to rest of the body. A healthy heart will have this process running smoothly, with a resting heart rate of 60-100 beats per minute.
There are many things that can cause an arrhythmia. These can include:
- Previous heart attack
- Coronary artery disease
- Changed structure of the heart due to certain conditions such as cardiomyopathy
- Diabetes
- Hypertension
- COVID-19 infection
- Hyperthyroidism
- Hypothyroidism
- Sleep apnea
- Certain medications such as drugs for treating cold and allergy
- Excessive intake of alcohol or caffeine
- Drug abuse
- Family history of arrhythmia
- Smoking
- Stress or anxiety
Risk factors
Those with any of the following factors face a higher risk of developing heart arrhythmia:
- Cardiac conditions: These include coronary artery disease, a history of heart surgery, thickened arteries, heart attack, injured heart valves, cardiac scars, and heart muscle disease.
- Hypertension: This disorder raises the risk of coronary artery disease and might cause the thickening and stiffening of the left ventricle, disrupting the function of electrical signals in the heart.
- Congenital heart disease: These conditions can affect the heart function such as rhythms.
- Thyroid disease: Thyroid hormone has a direct effect on the heart. Hyperthyroidism can increase the heart rate (tachycardia) as well as irregular heart rhythm. While hypothyroidism can cause a slow heart rate (bradycardia).
- Obstructive sleep apnea: causes irregular breathing while you are sleeping, which raises the risk of abnormal heart beating.
- Electrolyte imbalance: Chemicals in the blood such as potassium, sodium, calcium, magnesium, which regulate the electrical signaling of the heart. Arrhythmias can occur due to electrolyte abnormalities.
- Uncontrolled use of certain drugs and supplements: Many commonly used medications such as cough and cold medication can cause arrhythmia.
- Too much intake of alcohol: Alcohol can have effects on the electrical signals of the heart and put a drinker at risk of atrial fibrillation.
- Consumption of some drugs: People who consume caffeine, nicotine, or illegal drugs such as amphetamines and cocaine have a higher risk to developing heart arrhythmia.
Diagnosis
The diagnosis of heart arrhythmia start from history taking about signs and symptoms, reviewing the medical history or drug use, physical examination, and further can be confirmed by the following tests:
- Electrocardiogram (ECG or EKG): This procedure captures the heart’s electrical activity. Sensors (electrodes) are applied to the chest, wrists, and legs, then it is attached to the monitor to show the heart rhythm.
- Holter monitor: A doctor records the activities of the heart with this portable ECG during normal activities for at least 24 hours.
- Event recorder: Similar to a Holter monitor which records activities of the heart of a patient at times when symptoms appear and is generally required to wear the equipment for 30 days or until you have an arrhythmia.
- Echocardiogram: This is a non-invasive procedure which creates pictures that show the heart’s size as well as its structure and its movement.
- Implantable loop recorder: For patients with rare occurrences, the device will be implanted in the skin of the chest to detect any abnormalities of the heartbeats by persistently recording the heart’s electrical activity.
If any of these methods cannot detect arrhythmia, the doctor might trigger the arrhythmia with some other tests, including:
- Stress test: A patient is required to run on a treadmill while having the cardiac activity recorded and analyzed.
- Tilt table test: Lying down on a table before tilting the table to assess the changes of the heart rate, blood pressure and nervous system while the tilting angle is being changed. This test is generally recommended to those who are suffering from frequent fainting.
- Electrophysiological testing and mapping: This helps to locate where the arrhythmia is happening using catheters with electrodes at the tips, which are sent through the blood vessels to the heart. When the electrodes reaches the heart, they will show how the electrical impulses expand in the heart. The electrodes are also useful for stimulating the heart to beat at a certain rate that can trigger or stop arrhythmia.
Treatment
Only patients with severe type of arrhythmia or at risk of developing other heart conditions due to the disease are recommended to receive treatment which will be chosen based on what type of heart arrhythmia you have (tachycardia or bradycardia). Other patients may just require regular monitoring and checkups. There are many treatment approaches for heart arrhythmia, such as medications, vagal maneuvers, cardioversion, catheter procedures and cardiac surgery.
Medications
Medications will be based on the type of the arrhythmia and the possible complications. For example, your doctor will prescribe blood thinners if you have atrial fibrillation to prevent blood clots or certain medications to regulate the heart rate instead if you have tachycardia.
Therapies
- Vagal maneuvers: This approach might include the process of holding your breath and straining, dunking your face in ice water, or coughing. These activities helps to control the nervous system and slow down the heartbeat and are mostly recommended to those with supraventricular tachycardia that causes an abnormally fast heartbeat.
- Cardioversion: In this process, you will either be prescribed medications or receive a shock to the heart which is sent from paddles or patches on your chest to contain the abnormal electrical signals and normalize how your heart beat and is recommended for a few kinds of arrhythmia, including atrial fibrillation.
Surgery or other procedures
In some cases, catheter procedures or surgery might be required to implant a heart device to treat arrhythmia.
There are many procedures for the disease as follows:
- Catheter ablation: One or more catheters are delivered into the blood vessels before being guided to the heart. The surgeon will then use sensors at the tip of the catheter to create scars on the heart’s lining to block the irregular signals and make your heartbeat return to normal.
- Pacemaker: A doctor will implant small device around the collarbone’s area, sending electrode-tipped wires from the pacemaker into the blood vessels before guiding them to the inner area of the heart. The electrical impulses of this device help regulate the abnormal heart rate. This treatment is used for those with a slow heart rate, or bradycardias.
- Implantable cardioverter-defibrillator (ICD): The doctor will implant a battery-powered device in the collarbone’s area, with its electrode-tipped wires sent to the heart. Energy shocks, high or low, are emitted from the ICD to monitor the heart rhythm and fix any electrical abnormalities present in the heart. This device is mostly recommended to those at risk of severe heart arrhythmia, such as ventricular tachycardia or ventricular fibrillation, which affects the lower heart chambers.
- Maze procedure: This method is used to interfere with the abnormal heart signals that cause certain types of arrhythmia by making a pattern of scar tissue, called the maze, using heat or cold energy, or a scalpel, in the upper chambers of the heart. Maze procedure can interfere with heart signals as it does not send electrical signals. This is recommended for those who have not responded to other treatments or are scheduled for open-heart surgery for other disease.
- Coronary bypass surgery: This approach is effective for regulating the abnormal blood flow to the heart, recommended for those with both heart arrhythmia and severe coronary artery disease.




