Overview
Atrial fibrillation is a type of arrhythmia with chaotic and quick heartbeats in the heart’s upper chambers, or the atria. This disease causes the chambers to beat inconsistently with the lower chambers, or the ventricles, posing a risk of blood clots.
This disease can be either symptomatic or asymptomatic, and persistent or non-persistent. For some people, atrial fibrillation might cause palpitations, difficulty in breathing and fatigue.
In most cases, atrial fibrillation is a non-fatal disease. However, as it may pose a risk of stroke, heart failure and other heart-related defects, it can be a severe disease that needs to be treated to prevent any of these complications from occurring.
Treatment can include medications, cardioversion to restore a regular heart rhythm, and using a catheter to correct irregular heart electricity.
Symptoms
Some people with atrial fibrillation have no symptoms, but for patients with symptomatic atrial fibrillation, the symptoms include:
- Palpitations
- Irregular heartbeat
- Chest tightness
- Shortness of breath
- Dizziness
- Fainting
- Fatigue
The types of atrial fibrillation are as follows:
- Paroxysmal atrial fibrillation: The duration of symptoms varies from few minutes to hours, and symptoms can last for a week. It can happen occasionally and repeatedly, as well as can disappear on their own.
- Persistent atrial fibrillation: A patient with this type of the disease is recommended to receive treatment with medications or cardioversion as the symptoms do not disappear without being treated.
- Long-standing persistent atrial fibrillation: The symptoms are persistent in episode spans over one year.
- Permanent atrial fibrillation: This kind of atrial fibrillation cannot be permanently cured but can prevent the occurrence of blood clots and control heart rate with medications.
A patient is recommended to receive medical consultations in case of symptomatic atrial fibrillation. Immediate medical treatment is required for patients with a chance of having a heart attack, such as those suffering from chest pain.
Causes
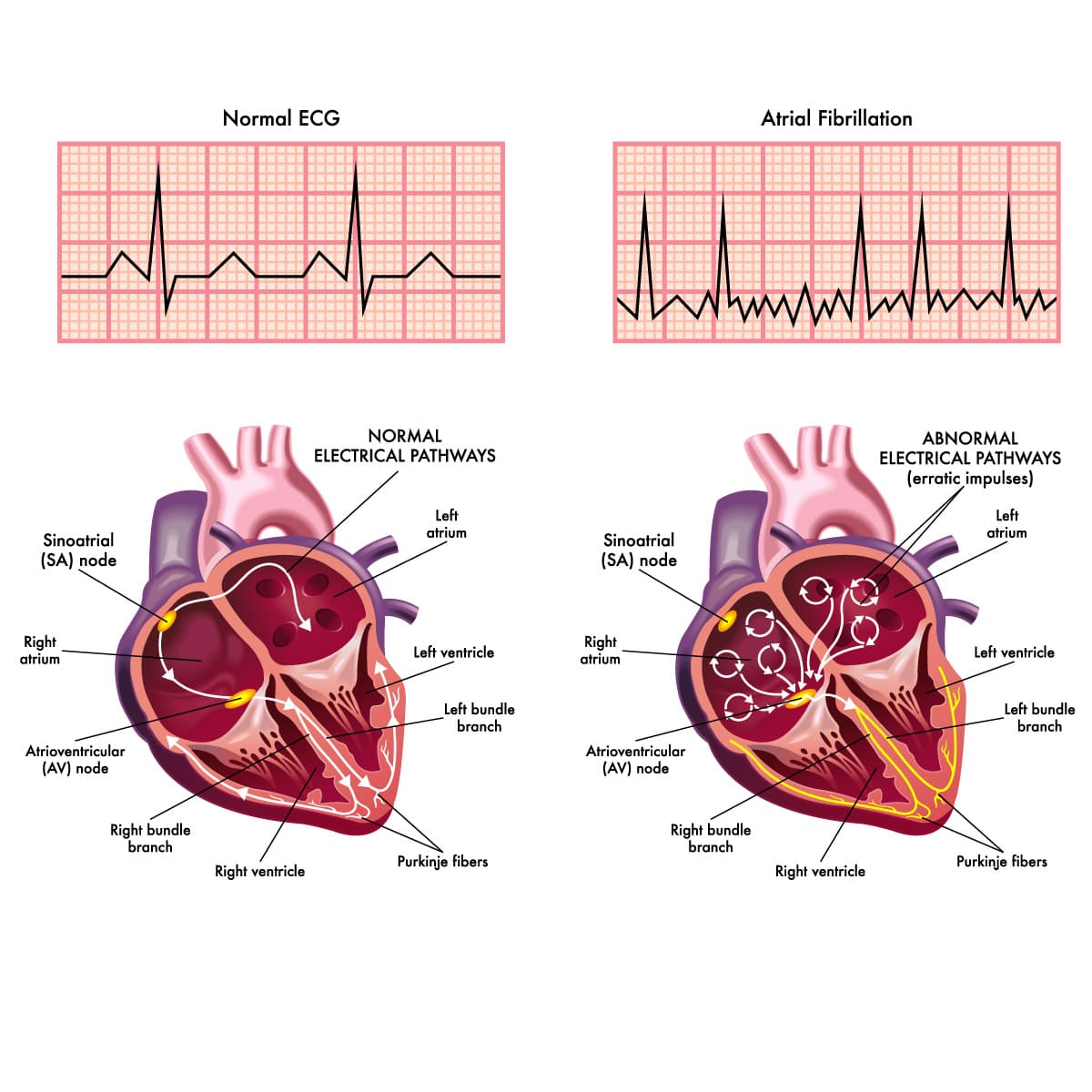
Atrial fibrillation is caused by irregular signals of the upper chambers of the heart, leading to quivers in the chambers causing the atrioventricular (AV) node, located between the upper and lower chambers, to be disrupted by many signals sent to the lower heart chambers. This cause the heart beat fast and irregular. Those with atrial fibrillation have a heartbeat rate of 100-175 beats per minute, higher than the normal rate of 60-100 beats per minute.
An abnormal cardiac structure is the most potential risk factor of atrial fibrillation. Other causes of the disease include:
- Coronary artery disease
- Myocardial infarction
- Congenital heart condition
- Valvular heart disease
- Hypertension
- Lung disease
- Having a history of cardiac surgery
- Sick sinus syndrome
- Sleep apnea
- Abnormal thyroid gland or metabolic issues
- Consumption of some stimulants or medications
- Viral disease
Despite symptoms, atrial fibrillation might not always cause heart issues or injury.
Risk factors
These following factors can raise the risk of developing atrial fibrillation:
- Age: The risk grows with age.
- Cardiac condition: A patient with any cardiac disease, previous heart attack or cardiac surgery.
- Hypertension: Hypertension, especially if not controlled by medication previously.
- Thyroid disease: Thyroid hormone has a direct effect on the heart. Hyperthyroidism can increase the heart rate (tachycardia) as well as irregular heart rhythm. While hypothyroidism can cause a slow heart rate (bradycardia).
- Chronic diseases: Diabetes, metabolic syndrome, kidney disease, lung disease and sleep apnea.
- Alcohol consumption: Alcohol can have effects on the electrical signals of the heart and put a drinker at risk of atrial fibrillation.
- Being obese
- Hereditary: Having a family member with atrial fibrillation.
Diagnosis
Some people are unaware that they have atrial fibrillation (A-fib). The doctor will use a stethoscope during examination to detect for abnormal heart rhythm in order to identify an A-fib or other heart disease.
There are many tests available to help a doctor diagnose atrial fibrillation or rule out other possible diseases that may cause similar symptoms to A-fib. The tests include:
- Electrocardiogram (ECG or EKG): This procedure detects irregularities of the heart rhythm. The doctor places electrodes on the chest, the arms and legs to monitor the cardiac electricity. The electrodes are connected to a computer to show results.
- Blood tests: A doctor may test the blood to find thyroid problems or substances that can cause atrial fibrillation.
- Holter monitor: A portable ECG device which monitors the patient’s heart beats for a period of at least 24 hours.
- Event recorder: Similar to a Holter monitor which records activities of the heart of a patient at times when symptoms appear and is generally required to wear the equipment for 30 days.
- Echocardiogram: It is a non-invasive test that creates images to see the size, structure and movement of your heart using sound waves.
- Stress test: requires a patient to run on a treadmill or stationary bike while the heart’s activities are being recorded.
- Chest X-ray: to check the condition of the heart and lung.
Treatment
A doctor aims to treat atrial fibrillation to reset the heart rhythm, bring the heart rate under control and prevent blood clots to reduce the chance of developing stroke.
Atrial fibrillation can be treated with these methods:
- Medications
- Cardioversion
- Surgery
Your doctor will choose the best treatment for you to put the disease under control and prevent severe complications, including strokes and heart failure.
Medications
A doctor will prescribe certain medications to make the heart beat slower and prevent severe complications like blood clots.
Medications used to treat atrial fibrillation include:
- Beta blockers: which control your heart rate when you are resting or doing an activity.
- Calcium channel blockers: which are used to put the heart rate under control but not recommended for patients with heart failure or hypotension.
- Digoxin: This medication is useful for controlling your heartbeat while you are resting. Digoxin is mostly required to be taken together with some other medications, such as calcium channel blockers and beta blockers.
- Anti-arrhythmic medications: are useful for both maintaining a normal heart rhythm and putting the heart rate under control but with more side effects compared to other heart rate-controlling drugs.
- Blood thinners or anticoagulants: which are prescribed to lower the risk of stroke and prevent blood clots and its effects on other organs. There are many types of blood thinners, such as warfarin, apixaban, dabigatran, edoxaban and rivaroxaban.
Cardioversion therapy
Cardioversion is a procedure to make a patient’s heart rhythm go back to normal and is recommended for those having symptoms of atrial fibrillation for the first time or being affected by the symptoms
There are two forms of cardioversion as follows:
- Electrical cardioversion: where paddles or electrodes placed on the patient’s chest are used to send electricity to the heart.
- Drug cardioversion: where drugs are delivered through an IV or orally to treat the disease.
Apart from emergency, a doctor might use cardioversion with patients for their scheduled treatment. In non-emergency treatment, a doctor might ask a patient to take a blood thinner such as warfarin for some weeks before cardioversion to prevent blood clots and strokes. When the treatment is finished, the patient may be required to take anti-arrhythmic medications to reduce the chance of the recurrence of atrial fibrillation.
Surgery or catheter procedures
A catheter procedure called cardiac ablation is recommended for those who have not responded well to other treatment options like medications.
In this procedure, your surgeon will insert a catheter into a blood vessel of the groin before guiding it to the heart. At the heart, the surgeon will create scars in your heart to block abnormal electrical signals and regulate your heartbeat. For ablation, the surgeon might use more than one catheter, with sensors on the tip, to create heat with radiofrequency energy or extreme cold to create the scars.
Alternatively, your surgeon might use a scalpel to perform ablation for open-heart surgery.
Atrial fibrillation can be treated with the following types of cardiac ablation:
- Atrioventricular (AV) node ablation: In this approach, your abnormal electrical signaling connection is destroyed with heat or cold energy applied to the heart tissue at the AV node. After finishing the treatment, the doctor will require you to wear a pacemaker for life.
- Maze procedure: The doctor uses this method to interfere with the abnormal heart signals that cause atrial fibrillation by making a pattern of scar tissue, called the maze, using heat or cold energy, or a scalpel, in the upper chambers of the heart. The maze can interfere with heart signals as it does not send electrical signals. If you are about to receive another cardiac surgery, such as coronary artery bypass surgery or heart valve repair, the doctor will recommend surgical maze procedure. This approach requires open-heart surgery as it requires the use of a scalpel to make the scars.
- Left atrial appendage closure surgery: used for patients who cannot take blood thinners. The procedure helps to prevent formation of clots in the left upper heart chamber by sealing a small sac, or an appendage, in the chamber. The left atrial appendage is closed by a closure tool guided to the sac with a catheter. The tool will be left there permanently after the catheter is removed.
Despite a successful cardiac ablation, there is still a chance of atrial fibrillation recurrence. In such case, a doctor may need to perform cardiac ablation or any other heart procedure again. A patient who has undergone cardiac ablation may be required to take blood thinners for life to prevent strokes.