Abdominal aortic aneurysm
Overview
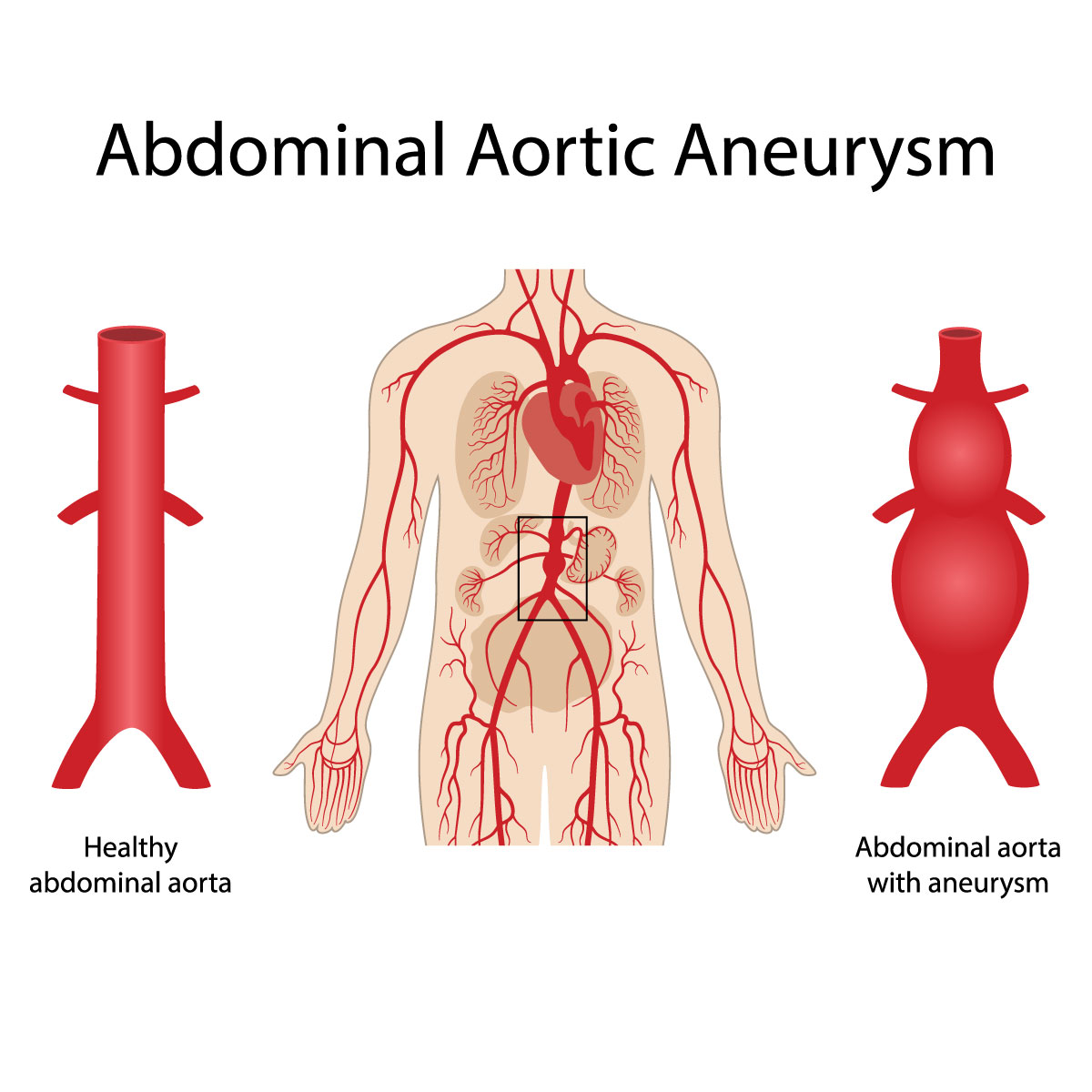
An aortic aneurysm is defined as abnormal widening or bulging of the wall of the aorta. The aorta is the largest artery that carries blood from the heart to the body. This is called an abdominal aortic aneurysm (AAA) when it happens in the part of aorta that is in the abdomen. The ruptured abdominal aortic aneurysm can cause fatal bleeding.
There are many treatments for abdominal aortic aneurysms, depending on the rupture’s size and the disease’s progression which include watchful waiting and emergency surgery.
Symptoms
Most patients with abdominal aortic aneurysm have no symptoms until the aneurysm is close to rupture, it may manifest the followings:
- Abdominal pain which is deep and persistent
- Back pain
- A pulsing sensation in the abdomen (similar to the heartbeat)
If you have any of these symptoms, seek emergency medical care immediately:
- Sudden or severe pain in the abdomen
- Shortness of breath
- Loss of consciousness
- Rapid heartbeat
Causes
An abdominal aortic aneurysm occurs in the abdominal part of the aorta. However, aortic aneurysm can be found in any part of the whole aorta. It can be caused by a variety of factors.
The disease-provoking factors include:
- Atherosclerosis: where the arteries get thickened due to buildups of fat and other substances inside a blood vessel.
- High blood pressure: which can damage and weaken the aortic walls.
- Blood vessel diseases: which causes inflammation of blood vessels.
- Bacteria or fungi-infected aorta: which rarely happens.
Risk factors
There are many risk factors for abdominal aortic aneurysms, including:
- Smoking: which is the high risk factor as it can weaken the aortic walls and increase the risk of developing aortic aneurysm and aneurysm rupture. The risk also depends on how many years you have smoked or chewed tobacco. Frequent male smokers aged 65-75 are recommended to have a one-time abdominal aortic aneurysm screening ultrasound in the abdomen to look for any risk of the disease.
- Age: as abdominal aortic aneurysms are most often found in people aged 65 and older.
- Gender: with abdominal aortic aneurysms more frequently found in men than women.
- Race: with white people being at a higher risk of developing the disease.
- Genetics: as having a family member who has or used to have abdominal aortic aneurysms increases the risk of developing the disease.
In case of being at risk of an aortic aneurysm, some other treatments might also be recommended, such as blood pressure medications which also help relieve stress on weakened arteries.
Diagnosis
In most cases, abdominal aortic aneurysms are found during a physical examination or a medical test done for another purpose, such as a heart or abdominal ultrasound.
The diagnosis of an abdominal aortic aneurysm starts from examining the patient’s body, reviewing the medical history and checking for any genetic risk. In case of suspecting an aortic aneurysm, the doctor will do imaging tests to confirm the presence of the disease.
Diagnosis tests for an abdominal aortic aneurysm include:
Abdominal ultrasound: by using sound waves to create real time images of the abdomen, including the abdominal aorta. A technician will performs an abdominal ultrasound by putting a slight pressure on an ultrasound probe (transducer) on the belly area before moving it back and forth.
Abdominal CT scan: which is painless as it uses X-rays to create cross-sectional images of the abdominal structures as well as clear images of the aorta. This helps determine the size and shape of an aneurysm. While the doctor is performing a CT scan, the doctor will ask you to lie on a table which slides into the scanning machine. The doctor might also inject contrast material into a vein to make your blood vessels show up more clearly on the images.
Screening for abdominal aortic aneurysm
Male frequent smokers are at a much higher risk of abdominal aortic aneurysm. The screening for this disease is generally recommended for the following groups:
- One-time screening using abdominal ultrasound for 65–75-year-old men who have a history of smoking
- 65–75-year-old men who have never smoked, but have a risk factor such as having a family member with a history of aneurysm
It has not been ensured if women aged 65-75 with a history of smoking or a family history of abdominal aortic aneurysm should receive abdominal aortic aneurysm screening. However, in general, disease screening is not required for non-smoking women.
Treatment
Abdominal aortic aneurysms are treated to prevent the aneurysms from rupturing through monitoring and surgery. The doctor will select the treatment based on the aneurysm’s size, progression of the disease, and location
Medical monitoring
Medical monitoring is mostly used for patients with a small abdominal aortic aneurysm without symptoms. In this medical process, the doctor will do regular checkups and imaging tests with the patient to monitor the disease’s progression as well as contributing factors, such as high blood pressure.
After a diagnosis is completed, doing an abdominal ultrasound every at least six months, with regular follow-up appointments, is generally recommended for those with a small abdominal aortic aneurysm which is not causing any symptoms.
Surgery
Those with abdominal aortic aneurysm of at least 5.0 inches in woman and 5.5 inches in man size are recommended surgery to treat the disease.
Abdominal aortic aneurysm repair surgery might also be recommended to those suffering from certain symptoms such as stomach pain or a leaking, tender or painful aneurysm in another area.
The size and location of abdominal aortic aneurysm are some of the factors used as well as general health to choose appropriate treatment option for the patient.
Abdominal aortic aneurysm surgery options include:
- Endovascular aneurysm repair (EVAR): is a minimally invasive procedure that can be done to treat abdominal aortic aneurysm by inserting metal mesh tube (graft) within the aneurysm through the groin arteries using X-rays to guide the graft into place. The graft will be expanded and fastened in place to strengthen the affected area of the aorta and prevent the aneurysm from rupturing. Anyway, not all abdominal aortic aneurysm is suitable for endovascular repair.
A patient is required to receive imaging tests from time to time after endovascular surgery to ensure no leakage in the grafted area. - Open abdominal surgery: is a procedure that remove the weakened part of the aorta and replacing it with a graft. A patient who receives this kind of surgery tends to fully recover within at least a month.
Both endovascular surgery and open surgery give a similar long-term survival rate.





